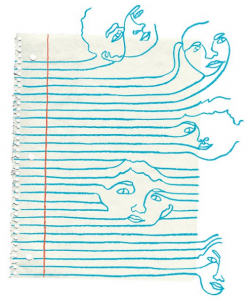
Distinct differences, striking similarities
Schizophrenia and Autism Spectrum Disorder (ASD) are both well-known developmental  disorders involving the brain. At first glance, the two seem strikingly different: when we think of symptoms of schizophrenia, we may think of hallucinations, delusions, or loss of speech and movement. With ASD, we may think of interrupted social and communication skills or repetitive behaviors. ASD is typically evident and diagnosed in childhood, while schizophrenia often doesn’t show up for several decades of a person’s life. However, the two disorders arise from similar molecular causes and even their symptoms are more alike than you might realize.
disorders involving the brain. At first glance, the two seem strikingly different: when we think of symptoms of schizophrenia, we may think of hallucinations, delusions, or loss of speech and movement. With ASD, we may think of interrupted social and communication skills or repetitive behaviors. ASD is typically evident and diagnosed in childhood, while schizophrenia often doesn’t show up for several decades of a person’s life. However, the two disorders arise from similar molecular causes and even their symptoms are more alike than you might realize.
Both disorders have a genetic component (meaning that children can inherit them from their parents) and an environmental component (meaning the circumstances a person grows up in from conception to adolescence influence their likelihood of developing the disorder). Let’s dive into the genetic and molecular component of these two disorders.
Schizophrenia on the brain
First, let’s look at the way schizophrenia is caused in the brain. It is a developmental disorder, meaning that the brain differences resulting in schizophrenia occur as the brain develops in the womb (even though symptoms usually don’t come about until later in life).
In a non-schizophrenic brain, an important signaling pathway (a cascade of events in a cell) known as the canonical Wnt pathway causes a protein called β-catenin to form and accumulate in neurons (brain cells). When there are high levels of this protein in a neuron, it causes certain target genes to be expressed. This means that the DNA of those target genes is copied and the proteins that the genes code for are made. The genes that are affected by β-catenin are important mostly during development, so the brain doesn’t need them to be at high levels all the time. A protein called GSK3 helps break down and recycle β-catenin so it doesn’t lead to gene expression all the time.
That was a lot of neurochemistry! If you’re interested in reading more, this paper by K. Singh dives even deeper into the pathway and its role in schizophrenia. If not, the big takeaway is that β-catenin is an important molecule during brain development, and GSK3 makes sure there isn’t too much of it. In schizophrenia, GSK3 is too active. This means that it breaks down more β-catenin than it should, so the genes making proteins needed for development aren’t expressed and the brain doesn’t form the way it’s supposed to.
 What about ASD?
What about ASD?
In ASD, the developmental disruptions resulting in brain changes are very similar. Even the exact same molecule is involved in the same way: β-catenin levels are too low, so genes that should be expressed during development aren’t, resulting in brain abnormalities. In ASD the lack of β-catenin is due to other interruptions to the signaling pathway, but the result is similar.
Can someone have both schizophrenia and ASD?
Yes; and it’s fairly common. When two disorders are frequently present together, the disorders are said to have high comorbidity. An individual’s official diagnosis could more likely be something like “ASD with psychosis”, but they would often display sufficient symptoms to be diagnosed with both disorders.
Additionally, studies have shown that individuals diagnosed with schizophrenia but not ASD still have higher levels of autistic symptoms than control groups. Symptoms of schizophrenia that are less-well known are often similar to characteristics of ASD: social withdrawal and exhibiting lower levels of emotion are two shared symptoms. These schizophrenia symptoms that are more similar or identical to ASD symptoms are called negative symptoms, not because they’re inherently bad, but because they exhibit a lack of something that is expected to be there, like emotional expression. The more well-known symptoms of schizophrenia like hallucinations and delusions are called positive symptoms because they’re adding something that doesn’t exist.
Conclusion
Despite very similar molecular causes involving a lack of the protein β-catenin during development, the differences between schizophrenia and ASD from age of onset to symptoms remain significant. However, knowing the similarities between molecular causes of the developmental disorders may help scientists in diagnosing and treating individuals exhibiting symptoms of both disorders in the future.
