The Link
Alzheimer’s Disease (AD) is the most common form of dementia diagnosed primarily in those older than sixty five and is thought to be caused by the build up of beta amyloid creating plaques and other build ups in the brain that cause neuron degeneration and death. Although this neurodegenerative disease affects over 50 million people world wide, a cure or general treatment has yet to be found. Although, two decades ago, scientists discovered an astounding link between dementia and diabetes. More specifically, between Alzheimer’s disease and type II diabetes. Those who develop type II diabetes will have an insensitivity to insulin which can often times be treated with insulin therapy and recommended exercise, diet change, and medication. The insulin pathway can become disrupted in patients who have Alzheimer’s disease, or those who have an insulin resistance, like in type II diabetes, may develop Alzheimer’s-like symptoms that can turn into actual dementia or AD. Currently, there are four mechanisms that connect Alzheimer’s disease to type II diabetes. This includes TNF-alpha mediated inflammation, unchecked PTP1B activity, deregulated mTOR signaling, and aberrant ganglioside metabolism. Here we will be taking a deeper look into PTP1B and the role it plays in both Alzheimer’s disease and type II diabetes.
The Modulator: PTP1B
It has been recently discovered that protein tyrosine phosphatase 1B (PTP1B) is an important modulator in the insulin pathway as well as in processes in the central nervous system, processes involved in Alzheimer’s disease. In the insulin signaling pathway, PTP1B negatively regulates the insulin pathway by directly affecting the receptor or by affecting down stream substrates (IRS 1/2). It also negatively affects leptin receptors and calcium channels. Over activation of PTP1B is most commonly caused by endoplasmic reticulum stress. Here is where Alzheimer’s disease can play a role in inducing type II diabetes. If a person has AD, there is most likely amyloid plaques present in their brain. These plaques are made up of an over abundance of
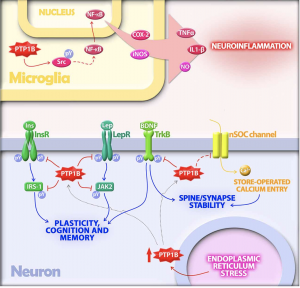
amyloid beta oligomers (ABOs). This over abundance can cause ER stress via neuroinflammation. So, ER stress over activates PTP1B which then goes on to over inhibit insulin signaling and receptors, leptin receptors, and calcium channels. If inhibition is present for long enough, a person can develop type II diabetes from the prevalence of insulin insensitivity, but they can also begin to develop worsened AD symptoms including synaptic plasticity and stability impairment and memory and cognition problems.
The steps described above explain how a person with AD can develop type II diabetes as well as progress the symptoms and severity of AD, but similar effects can be seen in a person who initially has insulin insensitivity. In this case, if a person develops type II diabetes from sources other than AD (unhealthy diet, overweight, environmental or genetic factors) and does not get treatment, the lack of insulin signaling can cause cognitive and memory deficits and synaptic plasticity impairment, both of which attribute to the diagnoses of Alzheimer’s disease. Then, if the symptoms become severe enough to where a person develops ABOs, the ER may become stressed increasing activation of PTP1B. No matter if a person is first diagnosed with Alzheimer’s disease or type II diabetes, it does not take much to get wrapped up into the cycle connecting the two diseases.
PTP1B Inhibition: a possible treatment?
Since PTP1B seems to be a problematic common denominator for both Alzheimer’s disease and type II diabetes patients, it seems reasonable to look here for a 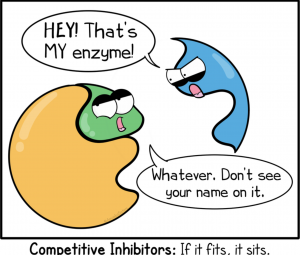 potential treatment for both diseases, and luckily, scientists are working on this! Inhibiting PTP1B would result in no or less inhibition of insulin signaling, leptin receptors, and calcium channels even under endoplasmic reticulum stress. This would help to decrease the chance of developing type II in AD patients as well as decrease any neurodegenerative symptoms caused by PTP1B caused inhibition. But, it has been deemed an extremely difficult task due to the fact that the active site on PTP1B that an inhibitor would attached to is shared by over 100 other “family members” of this molecule. This makes it difficult for the inhibitor to only effect PTP1B and not any other PTPs present in other parts of the body.
potential treatment for both diseases, and luckily, scientists are working on this! Inhibiting PTP1B would result in no or less inhibition of insulin signaling, leptin receptors, and calcium channels even under endoplasmic reticulum stress. This would help to decrease the chance of developing type II in AD patients as well as decrease any neurodegenerative symptoms caused by PTP1B caused inhibition. But, it has been deemed an extremely difficult task due to the fact that the active site on PTP1B that an inhibitor would attached to is shared by over 100 other “family members” of this molecule. This makes it difficult for the inhibitor to only effect PTP1B and not any other PTPs present in other parts of the body.
Fortunately, though, when PTP1B inhibitors have been administers peripherally they have been able to cross the blood brain barrier and have effects on the brain. A promising inhibitor that has been going through experimentation is that of CPT157633 and UA0713. In experimental trials these inhibitors have been shown to decrease the amount of PTP1B present in the brain. With continuous effort and research, scientists have the potential ability to create a PTP1B specific inhibitor that could help to alleviate symptoms of AD and type II diabetes or prevent one disease from triggering the other.