Figure 1; Picture Provided by Me
Alright, before you go any further in this blog post please just know that the information provided might make for an uncomfortable read. Now that you’ve been warned…. let’s begin. We’ve talked for a while now about schizophrenia and the underlying mechanisms that are related with the disease. In our conversations we’ve mentioned the side effects of antipsychotics; weight gain, dry mouth, constipation, hormonal imbalances, muscle twitches, etc. But it is important to look at the past and see where we have come as a scientific community. Treatments for schizophrenia have not always been so mild, if you can even consider the above side effects as being mild. Although I am a huge fan of imagery for learning I will not be including any images of many of the procedures that are listed. Reading about some of these things is distressing enough, seeing them seems unnecessary.
So, we are all probably aware that we require insulin to stay alive. As a reminder insulin acts on a tyrosine kinase receptor. Although we require insulin, more importantly we require regulated levels of insulin. If we receive excessive levels there is a potential that we could go into a coma. Medical professionals in the past thought that these comas had the potential to “jolt” someone out of their current mental illness. So, over the course of several weeks they would directly inject enough insulin to put someone into a coma, then after several hours they would administer glucose to bring their patients out of their induced state. Over the course of treatment, insulin levels would be increased until the staff felt that the treatment had reached its maximum “helpfulness.” What could go wrong when you induce 30-50 comas in the span of a month or two? Well of course the answer is a lot, some of the side effects included obesity, brain damage, and death, none of which sound overly pleasant to me. Sadly, even with extensive use of this treatment there was never any proof that inducing comas was an effective treatment method, yet the technique was used for quite a long time (JSTOR DAILY).
Wow, such a pleasant start to this blog post, let’s get into a slightly less appalling technique… the use of trephining, leucotomies, and lobotomies. Of course today we look at these techniques and consider them to be rather barbaric, although they did have the potential to erase behaviors attributed to schizophrenia. Trephining we are probably pretty familiar with, the surgery essentially boiled down to drilling a hole into someone’s head in order to “let out the demons!!!” I mean come on, of course that’s what drilling a massive hole into someone’s skull would do for them, there couldn’t possibly be any negative side effects. Below you can see the results of these surgeries, many of which people surprisingly survived (Faria, M., 2013). Sadly though there weren’t any improvements for the most part because demons are not known to actually reside in the skull. If there was improvement it was because the technique happened to damage brain tissue that coincidentally stopped the target behavior. Although it was never stated that these surgeries were done to schizophrenics one can assume that they were likely the victims of these procedures. “Madness” and “demons” are similar to voices and other positive symptoms of schizophrenia, there wasn’t a real definition for the disease until the end of the 19th century.

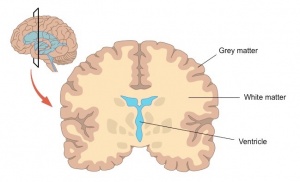
Leucotomies and lobotomies are very similar, just with a small difference between the two. Leucotomies focused on destroying the underlying white matter in the brain, while lobotomies were more focused on the prefrontal cortex and destroying the exterior grey matter (Faria, M., 2013). Look below for a visual representation of the separation between grey and white matter within the brain.
Although there is technically a distinction, lobotomies are usually thought of as the accumulation of both procedures. Interestingly enough leucotomies seem to have come before the lobotomy. Both leucotomies and lobotomies were performed initially using direct injections of alcohol into the target region in order to destroy brain matter. However, surgeons preferred to use a modified ice pick later on in the development of the surgery in order to directly damage the target region. It is actually super interesting to note that these doctors did actually have a method to their own madness. They would move their technique either posterior or anterior based on the illness that they were trying to treat. In some ways this does make sense, different regions of the brain are responsible for different behaviors. These surgeries did impact patients with schizophrenia, surgeons often noted that their patients had a much more flat personality, and that they did not have as many schizophrenia related symptoms (Faria, M., 2013). They would also note that after surgery these patients were easier to manage, leading one to ask the question, “were these surgeries out of necessity or because they were convenient for the facility.” These procedures essentially turned people into vegetables and assumed that these states were better than schizophrenia, a bold take. Just because something technically alleviates a problem does not mean that the end result is better.
Ok, now that we have discussed things that really don’t work at all, let’s talk about something that is still used today and quite useful. Electroshock therapy (ECT) is used to induce a seizure, which has been shown to relieve symptoms of mental illness. I don’t know exactly how, perhaps you could blog about it? ECT has serious benefits and is actually known to improve the lives of those that fail to respond to other treatments. The older equipment that was used is shown below.

Sadly however, ECT has a disturbing past. The technique was used to often as a punishment rather than a treatment, staff would administer ECT in order to control difficult patients and to maintain order in the hospital. Additionally, ECT did not use modern techniques in the past that make it safer today Although the following resources were technically available, for some reason those that conducted ECT procedures elected not to use any of them. There was no use of muscle relaxants to alleviate physical damage from the seizure itself, and no anesthesia was used to stop the pain from the actual shock. If that doesn’t sound pleasant enough, ECT was used for all of the wrong reasons in order to “cure” things that weren’t actually mental illnesses. A prime example of this would be the use of ECT to “treat” homosexuality (Sadowsky, J., 2017).
Okay so it is hard to sit here in my comfy chair and write about the things that were being done to those in the past. However, context is an important part of any intellectual conversation and I think it is important to include some now that we have concluded our conversation. The doctors and medical professionals of the time were in a real pickle, the mental hospitals were overflowing and they needed ways to help the patients who were otherwise never going to leave the systems that were in place to try and help them. Psychiatric medicine is not like it is today, there were so many people who were hospitalized for things that we can treat easily in modern times through the use of over the counter medications. Although it seems barbaric to us now, and frankly it was considered barbaric even in the past, the surgeons were trying to help even though they probably did more harm than good. Remember though that the individuals of the past did not know what we do now, we have the luxury of sitting here knowing as much as we do, only because of their trials and tribulations. The patients of the past suffered so that we can better treat those in society today.
The (unproven, deadly) common cure for … – JSTOR DAILY. (n.d.). Retrieved October 6, 2021, from https://daily.jstor.org/the-unproven-deadly-common-cure-for-schizophrenia/.
Faria, M. A. (2013, April 5). Violence, mental illness, and the brain – A brief history of psychosurgery: Part 1 – from trephination to lobotomy. Surgical neurology international. Retrieved October 6, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3640229/.
Phutane, V. H., Thirthalli, J., Kesavan, M., Kumar, N. C., & Gangadhar, B. N. (2011, April). Why do we prescribe ECT to schizophrenia patients? Indian journal of psychiatry. Retrieved October 6, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3136018/.
Sadowsky, J. (2017, January 13). Electroconvulsive therapy: A history of controversy, but also of help. Scientific American. Retrieved October 6, 2021, from https://www.scientificamerican.com/article/electroconvulsive-therapy-a-history-of-controversy-but-also-of-help/.
Treatment of schizophrenia. Treatment of Schizophrenia – an overview | ScienceDirect Topics. (n.d.). Retrieved October 6, 2021, from https://www.sciencedirect.com/topics/medicine-and-dentistry/treatment-of-schizophrenia.