Stats
In 2018, 139.7 million US adults were considered obese (CDC, 2021). This is an increase from 30.5% in 2000, to a whopping 42.4% in 2018 (CDC, 2021). To further break down these figures, 49.6% of Black adults, 44.8% of Hispanic adults, 42.2% of White adults, and 17.4% of Asian adults were considered obese in 2018 (CDC, 2021). Obesity prevalence is also correlated with socioeconomic status (SES) and amount of education received (CDC, 2021). Interestingly, men are least obese at the high and low ends of SES while women are least obese in only the highest SES (CDC, 2021). For more information, visit the CDC’s website here.
This high rate of obesity is destructive for many reasons. The most salient issue is directed at the obese themselves. Being obese can drastically increase one’s risk for cancer, heart disease, stroke, and type 2 diabetes (CDC, 2021). Additionally, the medical cost of obesity in the US impacts the obese, employers, and the government (through funding Medicare and Medicaid). The medical cost of obesity is estimated to be between $147 and $210 billion every year (GWU, 2013). So whether it’s for health of economic reasons, we should try to understand the underlying neurochemical cause of obesity.
Overview Of Science
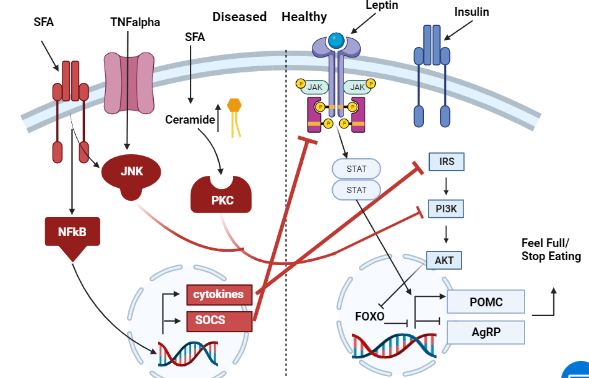
When trying to understand the neurochemistry of obesity, it is helpful to have a guide in front of you. To aid in your understanding, please refer to figure one below while reading the next section.
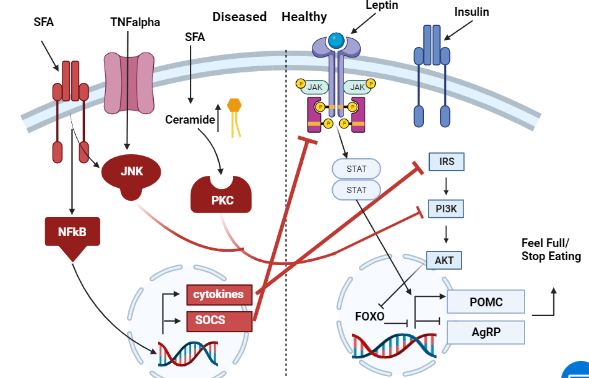
Figure 1: Obesity Pathway Artstract by Bretton Badenoch. The left side (red) shows some of the pathways that lead to dysregulation of hunger. The right side (in blue) demonstrates what neurochemistry looks like in a non-obese brain.First, we will take a look at the right side of figure 1. This side shows how appetite is controlled in a non-obese brain. Two of the most important molecules for controlling appetite are insulin and leptin. After eating a meal, insulin and leptin levels increase throughout the body. Insulin will then bind to an insulin receptor that ultimately causes an increased activation inproopiomelanocorticin (POMC) neurons and an inhibition of AgRP neurons (Jais, 2017). Leptin will have the same outcome, but acts on a separate leptin receptor (Jais, 2017). The decreased AgRP leads to depressed appetite while increased POMC activation promotes a feeling of fullness (Jais, 2017).
There are multiple ways for this pathway to go awry. Saturated fatty acids (SFA), and TNFalpha (a cytokine caused by inflammation) both contribute to the pathology of obesity through dysregulating hunger (Jais, 2017). The left side of figure one shows how these molecules interfere with POMC and AgRP activation leading to a feeling of hunger (Jais, 2017). This overactive feeling of hunger can lead to overeating and obesity.
Conclusion
Obesity is a disease that affects that affects nearly half of Americans (CDC, 2021). Because of this, it is a very costly disease both to the individual and society at large (GWU, 2013). Now that we know a bit of the neurochemistry underlying obesity, perhaps we can find more empathy for the obese. Obesity is often blamed on the individual for having weak willpower, but the chemistry shifts the blame to something beyond willpower. The connection between willpower and elevated levels of TNFalpha is tenuous at best.
It seems unlikely to me that willpower can decrease levels of inflammatory TNFalpha in any meaningful way. Rather, it’s possessing the knowledge on how to decrease levels of SFA and TNFalpha that seem most potent in preventing and reversing obesity. But that’s a topic for another blog post.
Citations
- CDC. (2021, September 30). Adult obesity facts. Centers for Disease Control and Prevention. Retrieved November 21, 2021, from https://www.cdc.gov/obesity/data/adult.html.
- George Washington University. (2013). Fast facts: The cost of obesity – George Washington University. Fast Facts Cost of Obesity. Retrieved November 21, 2021, from https://stop.publichealth.gwu.edu/sites/stop.publichealth.gwu.edu/files/documents/Fast%20Facts%20Cost%20of%20Obesity.pdf.
- Jais, A., & Brüning JC. (2017). Hypothalamic inflammation in obesity and metabolic disease. The Journal of Clinical Investigation, 127(1), 24–32. https://doi.org/10.1172/JCI88878