Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder with different levels of severity, characterized by its core symptoms involving deficits in social communication and interaction, restrictive and repetitive patterns of behavior and interests, and sensory abnormalities.[4] In more severe cases, symptoms can greatly impact an individual’s ability to perform everyday tasks including interpreting social rules, forming relationships, and managing stress. While there is no cure for ASD, early interventions in children with autism, such as behavioral therapy, can enhance their ability to function independently and support their development by teaching them important social and communication skills.
Prevalence:
It was estimated in 2023 by the CDC’s Autism and Developmental Disabilities Monitoring Network that 1 in 36 children had been diagnosed with ASD.[1] ASD affects males nearly four times more than females, and this gender difference has a major gap in ASD research. Symptoms generally appear in early childhood around the age of 2. However, there are individual variations and challenges with diagnoses and treatment. Individuals with higher socioeconomic status and better access to healthcare are found to be diagnosed earlier. Cultural knowledge should be researched further to assess healthcare access and how the process of getting help is impacted by stigmas and cultural values.
Etiology:
There is no single cause of ASD, and the spectrum of severity often comes from combinations of genetic changes and environmental factors. There are a lot of theories, however, about the etiology and pathogenesis of ASD: imbalances in excitatory-inhibitory neural activity; altered network connectivity (because of abnormal synapse formation, neuroinflammation, or oxidative stress), and altered social predictive coding that leads to sensory abnormalities. There are also many genetic mutations (SNPs and CNVs) that have been associated with ASD and examined in their impact on certain signaling pathways. With behavioral symptoms being the key descriptor and diagnostic criteria, various pathway dysfunctions are being looked at to create subgroups within ASD to improve individual treatment, the article we read this week focused on the dopaminergic system.
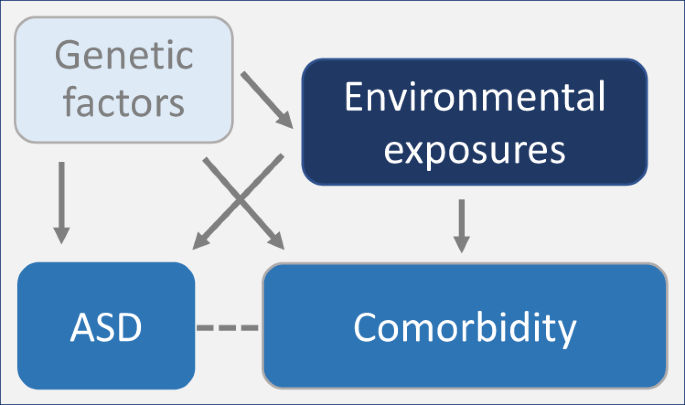
Figure 1. ASD etiology simplified to highlight the many connections and potential for comorbidities in future research looking at underlying causes.[2]
Comorbidities:
ASD has several comorbidities that are separated into 3 clusters: psychiatric (ADHD, OCD, anxiety, etc.), multisystem (gastrointestinal disorders), and seizures. The diagnosis of these comorbidities can be so closely related to ASD that their known underlying mechanisms are being researched as potential explanations of ASD as well. In the paper we read, they talked about ADHD in relation to dopamine signaling. In ADHD, there are disruptions caused by reduced dopamine transporters and D2 receptors in the nucleus accumbens and midbrain (brain regions that may be vulnerable in ASD).
Dopamine System:
Dopamine is a monoamine neurotransmitter produced in the substantia nigra and ventral tegmental area brain regions. It has a major role in learning and motivated behavior, which is why it could contribute to the underlying neurobiological mechanisms of ASD. However, there is no single cause of dopamine dysfunction that we can pinpoint either in ASD cases.
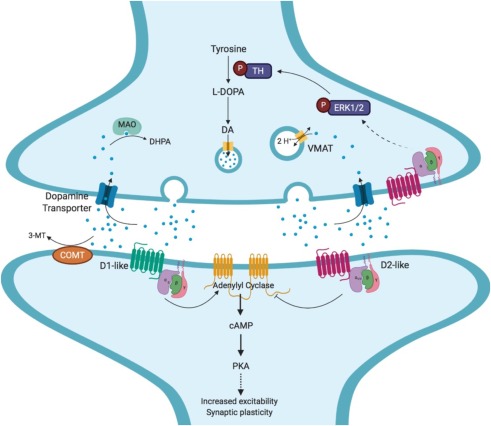
Figure 2. Dopamine signaling and its downstream functions that may be the connection to ASD – synaptic plasticity and development.[4]
Pharmacological Treatments?
Although there are currently two FDA-approved drugs used to treat irritable and aggressive behaviors associated with ASD, there are no pharmacological interventions approved to treat the core symptoms of ASD. Antipsychotics and SSRIs are the most prescribed to individuals with autism to treat the comorbid symptoms like anxiety. Further research is needed to test new drugs that could potentially target the core symptoms of ASD.
Figure 3. Common intervention strategies for individuals with ASD.[3]
Questions to leave with:
- How can we improve school systems to best help teach individuals with autism?
- How can we increase inclusion in jobs for individuals with autism?
- Should we consider comorbidities when creating subtypes?
- How do the various genetic risk factors cause the behavioral symptoms?
- How does diagnostic criteria play into the sex-based gap (what are the differences in symptom manifestations)?
