When we think of making everlasting memories, we often think of “the good” – road trips with friends, victories at athletic contests, adventuresome family vacations. If you’ve had such experiences, then recollecting these memories is likely to bring a smile to your face. But what happens when “the bad” becomes unforgettable? What happens when traumatic events or negative experiences become so ingrained in memory that day-to-day living becomes difficult? This is the reality for nearly 8 million adults every year, who suffer from a mental illness called post traumatic stress disorder (known as PTSD). There is no way to predict when trauma will happen, and for this reason there are no reliable ways to prevent the disease. Likewise, there are currently no end-all cures or treatments for this debilitating disorder, and the reason why some people develop PTSD and others don’t is still a scientific mystery. Nonetheless, recent research has shown some light on the ominous world of PTSD. In a world where people are exposed to war, crimes, and a variety of not-so-great experiences, finding new ways to help, support, and treat victims must begin with the basics – understanding the science behind what is unforgettable.
PTSD – A Mental Battlefield
One of the most relevant examples of PTSD in today’s world is the story of the returning soldier. The soldier returns after war overseas, reunites with family, and lives happily and safely at home for the rest of his life, right? Unfortunately, we are all too familiar with the reality that follows. Instead of living happily ever after, the soldier is startled at the sound of a shutting door, grows anxious from the revving of a car engine, or is shocked by the explosive nature of fireworks on the Fourth of July. Though not present in all soldiers, PTSD has been found to impact a notable portion of veterans, police, and first responders (all careers which can put someone in stressful situations). In essence, PTSD is a mental disorder that is triggered by either witnessing or experiencing an extremely stressful or traumatic event, such as warfare. Symptoms and implications vary in intensity, but among some of the most notable are:
- Severe anxiety
- Flashbacks, or reliving the event
- Unwanted memories of event
- Nightmares or dreams
- Avoidance of situations or discussions that might serve as reminders
- Some degree of depression, detachment, or feeling numb
- Insomnia
- Irritability
- Hypervigilance, being easily startled or frightened by “normal” events, sounds, images, etc (also called “stimulus generalization”)
Though PTSD patients often share similar symptoms as those with other stress and anxiety disorders, PTSD has recently been identified as its own “category” of mental disorders. For a full list of symptoms, risk factors, and advice on working with PTSD patients, visit, you can visit the Mayo Clinic webpage here.
Sufferers of PTSD often experience relationship problems and self-destructive behavior that interferes with daily life. It is often hard for victims to think about anything else, let alone anything positive. At this point, stress becomes pathological. Despite its severe implications, little is known in terms of how this stress disorder manifests itself in the human brain. What do the scientists think? Keep reading to find out!
When Memory Becomes Pathology
It’s very easy to get lost in the weeds of behavioral and psychological aspects of PTSD, but like every other mental illness, PTSD must start with a change in the brain. A quick read of this recent review paper offers potential explanations for a variety of factors that might contribute to such changes. The subjects can be quite confusing, and it can be hard to imagine how each piece fits into the big picture. It helps to keep one main question in mind when trying to describe such complicated processes:

What happens in the brain after a stressful event that turns a memory into pathologic symptoms?
We will begin by attempting to answer this question. Specifically, how does the brain change in response to stress, and why do such changes cause PTSD in some victims of trauma? To oversimplify things a bit, it boils down to mainly two things: epigenetics and gene expression.
- Gene expression refers to the process of converting DNA code into things (such as proteins and amino acids) our cells need to live, function, and carry out their specific tasks. Expressing different genes can lead to different outcomes or products.
- Epigenetics refers to changes or modifications in a cell that can alter gene expression, without changing the original DNA code itself.
How does this relate to PTSD? Research suggests that stressful events cause epigenetic changes inside neurons (brain cells) that alter gene expression and thus their function – and ultimately the brain’s function. There are multiple elements that work together to cause this change. A simplified proposed pathway of these elements is detailed below:
Stress → Stress Hormones, Glutamate Release → Epigenetic Change → Changes in Glutamate Transmission → Overexcitation, Changes in Learning, Brain Damage → PTSD
Looks complicated, doesn’t it? Let’s break it down step by step.
Stress and Stress Hormones: The word that every adult can relate to. Stress often comes with negative associations, and in the case of PTSD it’s no different. In the brain, stressful events (especially acute, traumatic events) trigger the release of stress hormones. These hormones are called corticosteroids and glucocorticoids. In addition, an increase in the amount of an excitatory neurotransmitter called glutamate is observed. This neurotransmitter tends to excite neurons, which is part of the reason why we are often awake and alert during stress! These increases are seen especially in parts of the brain necessary for emotion, memory, and fear – the limbic system. Notable parts include:
- Amygdala (fear, aggression, emotional learning)
- Hippocampus (memory consolidation and formation)
- Dentate Gyrus (part of the hippocampus, used when forming distinct memories)

Epigenetic Change: This step can be easiest understood by looking at a forced swim rat study. The test does essentially what it sounds like – it forces a rat to swim for a period of time. It serves as a means of eliciting a “traumatic” or stressful memory in a rat and seeing how the rat behaves afterwards. Essentially what happens is:
- Rat placed in water, forced to swim
- Rat grows stressed and frantically swims
- After a while, the rat goes still (called the immobility response, or learned helplessness)
- Rat is removed from water

Just keep swimming, just keep swimming…
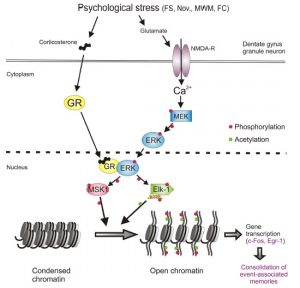
If the rat remembers this traumatic experience, then it will grow immobile in a shorter amount of time if placed in another forced swim test, having remembered what happened in the previous test. Interestingly, scientists found that an epigenetic change is responsible for the formation of this memory, and the development of the immobility response. Using a method called chromatin immunoprecipitation, or CHIP (not the edible kind), scientists were able to look at changes in chromatin (genetic material within cells) following a stressful event. The chemical change that literally “marked” the formation of this strong memory was found in a protein, called a histone (conveniently named H3s10KM), in the dentate gyrus. Here’s the chemical rundown:
- Stress hormones bind to stress hormone receptors in brain cells, creating complexes
- Meanwhile, glutamate interacts with its own receptors, called AMPA and NMDA receptors, normally important for long term memory formation. More basic information about this can be found here
- Calcium moves into the cell through NMDA. This leads to chemical changes that activate a series of enzymes (called MEK and ERK, specifically – scientists are really good at giving names!)
- ERK interacts with stress hormone receptor complexes
- This interaction leads to a phosphate “on switch” being added to (you guessed it) more enzymes. The one we are interested in here is called Elk.
- After being exposed to a particular electric signal from a brain cell (called p300, in response to the stressor), Elk adds a chemical group called an acetyl to the histone.
- Adding an acetyl to this histone “opens” the cell’s DNA at some particular genes (formally known as immediate early genes), which makes it easier for them to be reached and expressed. These genes have been found to regulate stress responses.
Interestingly, using chemicals that block the development of this acetyl “mark” or made the patheay malfunction led to rats that panicked every time they were placed in a similar situation, similar to what is observed in PTSD patients. If you’re more of a visual learner, here’s a helpful figure from the text:
Changes in Glutamate Transmission and Brain Damage: Seems like quite the process doesn’t it? If you haven’t stressed yourself out reading about epigenetics yet, here’s what happens next. The particular function of these “exposed” genes isn’t exactly known, but it’s predicted that they can change glutamate release throughout the limbic system, and this might lead to higher levels of glutamate in these parts. If you read the article linked above, you’ll know that glutamate is normally considered “the good stuff” – it helps with learning via interaction with AMPA and NMDA receptors and getting neurons all fired up! Normally, glutamate helps learning by activating a process that recruits more AMPA receptors to neurons (in a region called a synapse, these are what we think of when we hear “neuron connections, but it’s actually an empty space!). These receptors make it easier for neurons to respond to incoming signals. This explains why rehearsing something over and over makes it easier to remember – your neurons respond more easily to an incoming stimulus! But like the mantra goes, too much of a good thing isn’t great. So what happens if there’s too much glutamate? In a nutshell:
- Neurons may become overexcited
- Too much glutamate accumulates and becomes toxic
- Can promote epigenetic change, which messes with the gene expression mentioned above, enhancing the cycle and stress responses
- Hyperactive recruitment of AMPA receptors may strengthen memory of the stressful event
- Too much stimulation in the limbic system can lead to anxiety, insomnia
- An overactive amygdala can “overwork” the hippocampus (which tries to “calm it down”), leading to damage in this area of the brain
- Damage to the dentate gyrus leads to loss of ability to distinguish distinct memories from each other, which can lead to fear and anxiety from what we’d consider “normal” events
- Symptoms of PTSD manifest

The bottom line: like most things in life, glutamate is best in moderation. At such dramatic levels, which can result from being exposed to a traumatic event, the making of a memory truly becomes a potentially harmful pathology.
Victory for Victims – Treatments for PTSD and the Future

Although we are far from finding an efficient, effective pharmacologic treatment for PTSD, the paper above details some existing research done on animal models to study behavior that stems from learning and memory. Studying the behavior of rats in response to administering specific drugs that target the mechanisms described previously offers us a look at what works and what doesn’t. Currently, drugs often used to treat other mental disorders can be used to treat the symptoms of PTSD. These include
- Antidepressants
- Anti-epilectic medication
- Anti-anxiety medications
- NMDA antagonists (only tested in the lab, and not safe for healthy individuals)
Sadly, there aren’t many approved medications for treating PTSD, due to the sheer number of undesirable side effects. The most successful modern treatment for PTSD is not chemical – it’s largely based on behavioral therapy. Research on animal models has even found that something as simple as exercise can lessen symptoms of this disorder! But having PTSD also doesn’t spell out the end. Many PTSD patients are able to improve their symptoms to some extent, and some even make significant steps towards full recovery. When brainstorming modes of prevention though, there is one big question that looms overhead…
How stressful does an experience have to BE to trigger PTSD?
The true answer is we don’t know – and we might never. Why do only some victims of trauma develop PTSD? We don’t know. Memory formation is an extremely complicated topic in itself, and how we respond to and perceive our memories varies from person to person, rat to rat. How the brain decides what is stressful enough to literally “leave a mark” and what is so insignificant we won’t even notice is beyond our understanding. The brain in itself, like PTSD, is a mysterious object in science. Nonetheless, how we act depends on what we remember.
