TBIs & Tau
Traumatic brain injuries (TBIs) are high impact forces that cause changes in brain function. Even mild TBIs effect the brain, and without proper recovery, lead to devastating effects. One of the main changes that occurs in the brain after TBIs is how the protein tau is regulated. Tau is crucial in maintaining the structure of brain cells (microtubules) and allowing them to signal properly (3). TBIs effect tau’s binding to microtubules by causing an increased level of phosphate binding to tau, destabilizing signaling (2). The brain has ways to identify these flawed proteins and degrade them, but this mechanism is also damaged by TBIs. These hyperphosphorylated tau proteins form clumps (aggregates) separate from the microtubules, seen in figure 1.
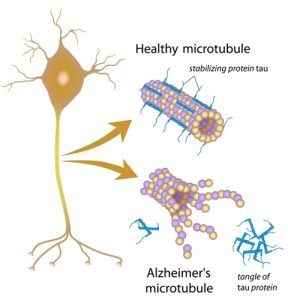
Figure 1: Healthy microtubules are stabilized by tau proteins whereas microtubules in those with Alzheimer’s don’t have this stabilization. Instead tau proteins become tangles separate from the microtubule (image from https://alzheimersnewstoday.com/news/tau-protein-leads-to-neuronal-death-in-alzheimers/).
Disease & Difficulties
Unfortunately, over 5 million people in the United States are currently living with neurodegenerative diseases resulting from TBIs. Dysregulated tau proteins play a major role in causing these devastating effects. The tau aggregates that form develop into neurofibrillary tangles (NFTs), which multiply and spread throughout the brain (5). These NFTs are linked to severe tauopathy neurodegenerative diseases, such as Alzheimer’s and CTE. This video shows the process of tau forming these NFTs.
As with all TBIs, these changes in the brain are incredibly difficult to detect and predict effects of until it is too late. A range of factors, such as age, severity of injury, genetics, and recovery time and methods, contribute to how an individual’s brain is effected and can rebound. Prevention and early intervention are weak areas across all long term diseases associated with TBIs. Research gaps include how to target and counteract tau dysregulation and how to repair the damage it causes.
Success in Science
Therefore, current scientific research is working to bridge these gaps in research. They have had lots of success on this topic, using tau as a tool for diagnostic tests. By detecting levels of the hyperphosphorylated tau protein, medical experts can estimate the levels of NFTs in the brain to accurately diagnose Alzheimer’s disease (6). They have also found PET scans (shown in figure 2) to be useful in detecting the progression of neurodegeneration in the brain. These scans detect the levels of NFTs and show where they are concentrated in the brain. If a TBI occurred, the area of impact will be where the NFTs are most concentrated (4).
These advances are useful in diagnostics and monitoring neurodegeneration, but lack use in prevention or repair. Research on TBIs, tau, and all neurodegenerative disease are ongoing. Future directions in science would lead towards earlier detection of tau dysregulation, genetic factors correlating with the brains resilience, and TBI prevention methods that would better reduce the risk of neurodegeneration diseases.
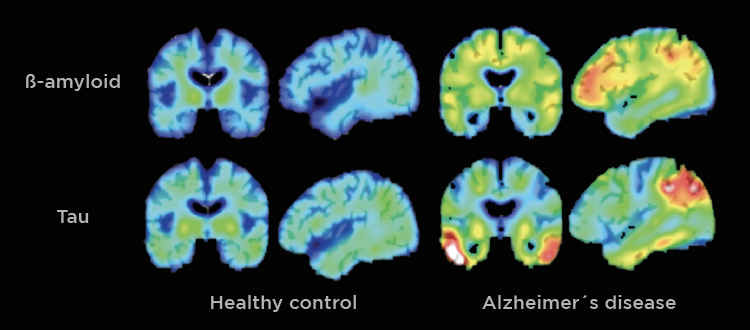
Figure 2: Healthy brains show consistent imaging throughout whereas Alzheimer brains show clear hot spots where NFTs are concentrated (image from https://danielleal.pt/en/sleep-deprivation-and-alzheimers-disease/).
Conclusion
TBIs can have devastating impacts within the brain that may go unnoticed until long-term heath symptoms reveal themselves. Tau dysregulation, specifically, damages brain stability, communication, and cognitive ability leading to neurodegenerative diseases. Though neurovegetative diseases are becoming increasingly common, scientific research and application are working to protect against the effects of TBIs and better repair the damage they cause.
More information about the various effects TBIs have on the brain can be found in this research: 2014 The_New_Neurometabolic_Cascade_of_Concussion.3(1) (1)
References
[1] Chauhan N. B. 2014. Chronic neurodegenerative consequences of traumatic brain injury. Restorative neurology and neuroscience, 32(2), 337–365. https://doi.org/10.3233/RNN-130354
[2] Giza, C. C., & Hovda, D. A. 2014. The New Neurometabolic Cascade of Concussion. Congress of Neurological Surgeons. https://doi.org/10.1227/NEU.0000000000000505
[3] Guo, T., Noble, W., & Hanger, D. P. 2017. Roles of tau protein in health and disease. Acta neuropathologica, 133(5), 665–704. https://doi.org/10.1007/s00401-017-1707-9
[4] Jie, C., Trayer, V., Schibli, R., & Mu, L. 2021. Tauvid: The First FDA-Approved PET Tracer for Imaging Tau Pathology in Alzheimer’s Disease. Pharmaceuticals. 14. 110. 10.3390/ph14020110.
[5] Martin, S. P., & Leeman-Markowski, B. A. 2024. Proposed mechanisms of tau: relationships to traumatic brain injury, Alzheimer’s disease, and epilepsy. Frontiers in neurology, 14, 1287545. https://doi.org/10.3389/fneur.2023.1287545
[6] Schneider T. 2025. Highly accurate blood test diagnoses Alzheimer’s disease, measures extent of dementia. WashU Medicine. https://medicine.washu.edu/news/highly-accurate-blood-test-diagnoses-alzheimers-disease-measures-extent-of-dementia/#:~:text=In%20the%20study%2C%20the%20researchers,Alzheimer’s%20disease%20progression%20from%20blood
