Rest after a Traumatic Brain Injury is not just about symptom relief. It’s a vital biological process that allows the brain to repair itself. Without rest, the brain remains in a vulnerable state where healing systems cannot function properly. A main factor that influences this vital rest period is age. [1]
The Brains Quiet Recovery
The brains repair process occurs quietly, on an ionic level, making it difficult to completely determine when someone is back to normal. Recovery doesn’t end when symptoms fade. [2] There is a common blanket statement often told that rest is important the first 24-48 hours post brain injury. [3] This recommendation is supported by current concussion management guidelines. A brain cannot operate on a universal recovery timeline and happens differently in every individual. Some neural systems may stabilize quickly, while others remain the same or even decline.[4] This provokes the question of if we can’t see brain recovery, how do we decide when someone is truly healed?
The topic of rest after a mild Traumatic Brain Injury is still being researched because of all the complexities involved. It’s particularly difficult because a TBI occurs invisibly and standard brain scans can look normal even after a severe injury. [5]
Instead, clinicians rely on cognitive and behavioral assessments such as the Glasgow Coma Scale. It is used to assess a person’s level of consciousness after a brain injury. There is also The Rancho Los Amigos (RLA) Cognitive Scale which uses a 10 level assessment to measure recovery. These tools are useful early on but it does not measure subtle cognitive changes that characterize recovery from mild Traumatic Brain Injury.
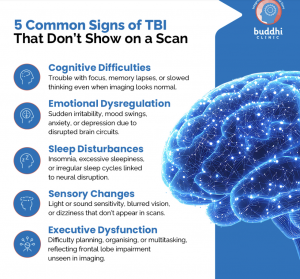
This image was source from Buddhi Clinic
The Role Age Plays
Recent findings on Brain blood barrier disruptions across all ages and the biology of rest help explain why recovery timelines of recovery vary so widely. After a traumatic brain injury, the brain undergoes a metabolic cascade. This cascade generally follows the same pattern, however the duration and intensity of these disruptions in the brain are unique to each person.[4]
A longitudinal study conducted by Marquez de la Plata CD et al. found that older patients show greater decline in the first 5 years after a TBI while the most improved were the youngest patients. [6]
Limited understanding of TBI recovery can cause people to ignore recommendations to rest while also contributing to under-diagnosis thereby having negative effects including a reduced quality of life and even death. [7] Therefore, it is vital to promote individualized recovery rather than a one-size-fits-all recommendation. Increasing understanding of recovery post TBI can also help to develop age related recovery guidelines. This understanding of recovery affects how people make decisions at school, work and in healthcare.
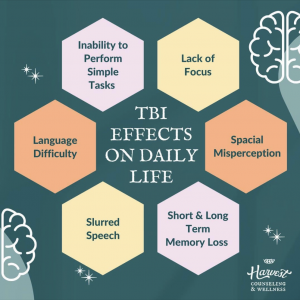
The most important thing to remember about a traumatic brain injury is that recovery doesn’t end when symptoms fade. After a concussion, the brain is quietly working to restore its protective barriers and reduce inflammation. Returning to school or work too quickly can prolong symptoms or increase vulnerability to re-injury. Rest isn’t an optional pause- it’s the biological window that makes recovery possible.
Diagram sourced from Harvest Counseling and Wellness
ChatGPT was used in the formation of this post
-
de la Plata, C. M., Hart, T., Hammond, F. M., Frol, A., Hudak, A., Harper, C. R., O’Neil-Pirozzi, T., Whyte, J., Carlile, M., & Diaz-Arrastia, R. (2008a). Impact of age on long-term recovery from traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 89(5), 896–903. https://doi.org/10.1016/j.apmr.2007.12.030
-
Wilson, L., Stewart, W., Dams-O’Connor, K., Diaz-Arrastia, R., Horton, L., Menon, D. K., & Polinder, S. (2017). The chronic and evolving neurological consequences of traumatic brain injury. The Lancet. Neurology, 16(10), 813–825. https://doi.org/10.1016/S1474-4422(17)30279-X
-
Guidelines for recovery. (n.d.). Concussion Alliance. Retrieved February 10, 2026, from https://www.concussionalliance.org/recovery-guide
-
Giza, C. C., & Hovda, D. A. (2014). The new neurometabolic cascade of concussion. Neurosurgery, 75(Supplement 4), S24–S33. https://doi.org/10.1227/NEU.0000000000000505
-
Lee, B., & Newberg, A. (2005). Neuroimaging in traumatic brain imaging. NeuroRx, 2(2), 372–383. https://doi.org/10.1602/neurorx.2.2.372
-
Marquez de la Plata, C. D., Hart, T., Hammond, F. M., Frol, A. B., Hudak, A., Harper, C. R., O’Neil-Pirozzi, T. M., Whyte, J., Carlile, M., & Diaz-Arrastia, R. (2008). Impact of age on long-term recovery from traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 89(5), 896–903. https://doi.org/10.1016/j.apmr.2007.12.030
- National Academies of Sciences, E., Division, H. and M., Services, B. on H. C., Policy, B. on H. S., Care, C. on A. P. in T. B. I. R. and, Matney, C., Bowman, K., & Berwick, D. (2022). Traumatic brain injury prevention and awareness. In Traumatic Brain Injury: A Roadmap for Accelerating Progress. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK580082/
