Just This Once
Think back to those college days of little responsibility and too much fun. Some of us were so caught up with our desire to “fit in” and be “cool,” that when offered a drink of alcohol or a “hit” of some drug, we simply could not refuse. Many of us probably thought to ourselves, “It’s not a big deal; after all, it is just this one time.” Or is it?
I have never personally connected addiction to neurochemistry, but rather I have always associated addiction with personal choice. It has also never occurred to me that one could become addicted to alcohol or drugs after one single, potentially innocent exposure. Through the study of current neurochemistry research, I have been awakened to the reality that addiction is neurological, NOT personal choice. Addiction has implications in the neurological wiring of our brains that metaphorically TRAPS us in the never-ending cycle of cue exposure, craving, and relapse.
Dopamine: My “Feel Good”
Dopamine, a neurotransmitter involved in reward-motivated behavior, is released in the brain when we partake in something pleasurable, whether that be drugs, alcohol, food, or sex. The dopamine concentration within the brain needs to be regulated in order to ensure proper functioning, which is the main problem in addiction.
There are many types of dopamine receptors in the brain that undergo various biochemical reactions when dopamine binds, but D1 and D2 receptors are of particular importance in the brain’s reward pathway:
D1: Direct reward pathway activation; lower affinity for dopamine (activated by high concentrations of dopamine)
D2: Indirect punishment/aversion pathway inhibition; higher affinity for dopamine (activated by low concentrations of dopamine)
When taking drugs or alcohol, dopamine is released in central brain regions, specifically the nucleus accumbens (NAc) and the ventral tegmental area (VTA). In response to a drug cue or drug itself, dopamine neurons in the VTA cause a rapid increase in dopamine release from the NAc. This rapid type of dopamine release causes stimulation of both low-affinity D1 and high-affinity D2 receptors. When both of these receptors are activated you receive maximal reward (“feel good” feeling), because the D1 receptors stimulate reward feelings and D2 receptors are inhibit/block feelings of aversion
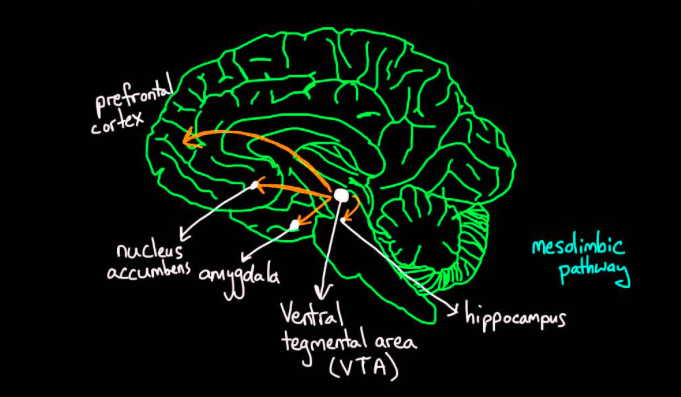 Figure 1. Reward circuitry in the brain.
Figure 1. Reward circuitry in the brain.
Trapped
Depending on various factors (genetics, age, type of drug, etc.), one could become addicted after their first substance exposure, or may never form an addiction even after numerous uses. When you abuse substances and dopamine is released in significant quantities in the brain, the high-affinity D2 receptors become overstimulated. Over time your body tries to regulate this overstimulation by lessening the number of D2 receptors in the brain. This requires you to take more of a drug or drink more alcohol in order to achieve the same maximal reward and “feel good,” also known as tolerance. This down-regulation of D2 receptors also leads to a lack of prefrontal cortex stimulation (responsible for decision-making), and thus a decrease in self-control and an increase in compulsive behavior.
During drug or alcohol use, the brain creates reward circuits and strengthens connections with the hippocampus (memory center) and amygdala (emotion center). Due to these connections, drug and alcohol use are associated with “cues,” such as a specific location, person, or time of day. These cues remind you of using drugs or alcohol, and when exposed to these cues, dopamine is released within the VTA and NAc, giving you that CRAVING feeling we all know far too well. The strong, built-up neural connections in the reward pathway associated with the abused drug(s) or alcohol TRAP you inside of a cycle of craving and impulsive behavior that ultimately lead to relapse.
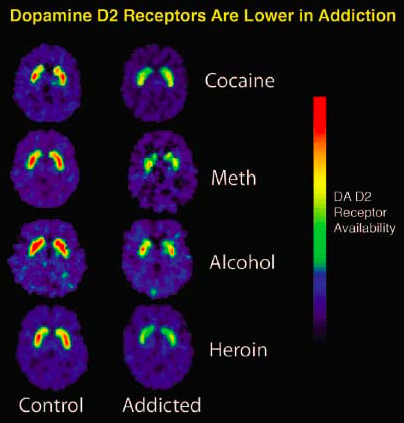 Figure 2. Dopamine D2 receptor availability in healthy brain vs. substance abuse brain.
Figure 2. Dopamine D2 receptor availability in healthy brain vs. substance abuse brain.
Addiction Relief?
Can one ever escape from this viscous cycle? The neural connections in the reward pathway associated with abused substances are strong and do not disappear rapidly, even after the cessation of substance use. Currently, there is minimal research on whether the brain is able to restore itself to normal circuity after one ceases from using the previously abused substance. Brain stimulation is at the forefront of addiction treatment research, but has yet to be approved by the FDA due to many associated risks and side-effects. If there is one thing that you take away from this blog, it would be that addiction is NOT a personal choice, it is a neurological disorder, one that is relentless and extremely difficult to treat. So next time someone offers you a “hit” or a “pull,” think twice.
For more information on the neurochemistry of addiction, please visit:
http://www.cell.com/cell/fulltext/S0092-8674(15)00962-9
Featured Images from:
https://www.khanacademy.org/science/health-and-medicine/mental-health/drug-abuse-and-drug-addictions/v/reward-pathway-in-the-brain
http://www.edinformatics.com/news/drug_addiction_treatment.htm
