Understanding the Fog of Alzheimer’s Disease
It is inevitable that we all grow old. There is nothing we can do to reverse the cruel effects of time. One of the most common effects of old age is Alzheimer’s disease. This horrible disease causes more than just one person to suffer from its effects. Family and friends of the patient have to deal with their loved one not remembering details about them or even that they exist. But what causes our loved ones to lose their memories? Researchers are not sure where the disease originates exactly, but there is knowledge about what happens once the disease develops.
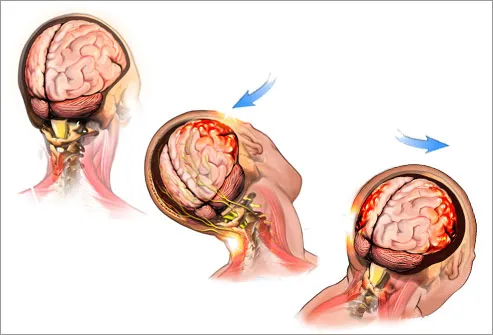
Some people have heard of the plaques and tangles involved in Alzheimer’s but they may not know what they actually do within the brain. This figure depicts the problems in the neurons of Alzheimer’s disease. The right side shows how a normal brain should work. Insulin in the brain binds to the insulin receptors which activates a pathway called PI3K/Akt. The activation of Akt leads to several important cell functions. In Alzheimer’s, plaques made of built up Aβ have the ability to remove insulin receptors from the cell membrane and tangles of phosphorylated tau protein lead to cell death. Because the receptors are being taken out of the membrane, Akt is not able to inhibit the activation of GSK3β, so more tau is phosphorylated and more tangles are produced.
 http://journal.frontiersin.org/article/10.3389/fnins.2015.00204/full
http://journal.frontiersin.org/article/10.3389/fnins.2015.00204/full
Another lesser known way the cell function is altered in Alzheimer’s is with two proteins called FOXO and mTOR. FOXO is a transcription factor and mTOR plays a key role in the PI3K/Akt pathway. When we age, our cells are generally undergoing some elevated levels of stress. In order to correct the cell’s function from the stress, FOXO needs to have high activity and mTOR needs low activity. In Alzheimer’s, FOXO levels are low and mTOR levels are high so the response to the stress is not reversed.
 http://www.sciencedirect.com/science/article/pii/S053155651300065X
http://www.sciencedirect.com/science/article/pii/S053155651300065X
It is unclear where in this system the Alzheimer’s begins, but it is clear that once it begins, there is a snowball effect making the disease become worse with time. At the time, there are no medications that prevent or cure Alzheimer’s, but there are some to help the symptoms. Hopefully with further research, a source of the disease will be found or an early diagnosis system will be discovered with an early treatment to prevent symptoms. In my opinion, Alzheimer’s is one of the most awful diseases. Even though it doesn’t have many physical symptoms, the loss of memory is hard for not only the patient but also for the family and friends.