Imagine a world where you never know what the person next to you is thinking or how they’re feeling. Imagine attending social events or new experiences that are supposed to be exciting and fun but instead cause you debilitating stress and anxiety. Imagine being so overwhelmed and overstimulated by loud, bright, or crowded environments that you lose control of your body and begin to panic. Imagine the frustration, isolation, and confusion that these daily challenges would bring. For someone with autism spectrum disorder, they don’t need to imagine – this is their reality.
ASD: A “Puzzling” Disorder
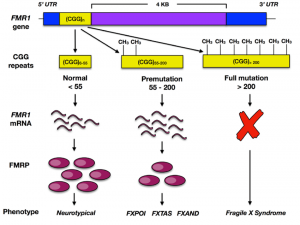
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that causes problems with social communication and interaction, affecting about 1 in 36 children[1]. People with ASD often have restricted or repetitive behaviors or interests and may have abnormal patterns of movement. Autism can be diagnosed at any age, but it is described as a “developmental disorder” because symptoms usually emerge in the first two years of life[2]. Known as a spectrum disorder, there is a wide range of symptoms in people diagnosed with ASD. While autism is widely prevalent and the symptomology is generally understood, the exact cause of the disorder is unknown, and consequently, there is no cure for ASD. This is due to the heterogeneity of the disorder; many genetic and environmental risk factors likely contribute to a wide variety of symptoms. Recent research, however, may have unlocked a piece to the complex puzzle of ASD development and possible treatment directions. In this blog post, I will highlight the recent work on dopamine dysfunction in ASD, shedding light on what could be a successful avenue for improving the quality of life for those with ASD.
Dopamine: A Key Piece in the Neurochemical Puzzle
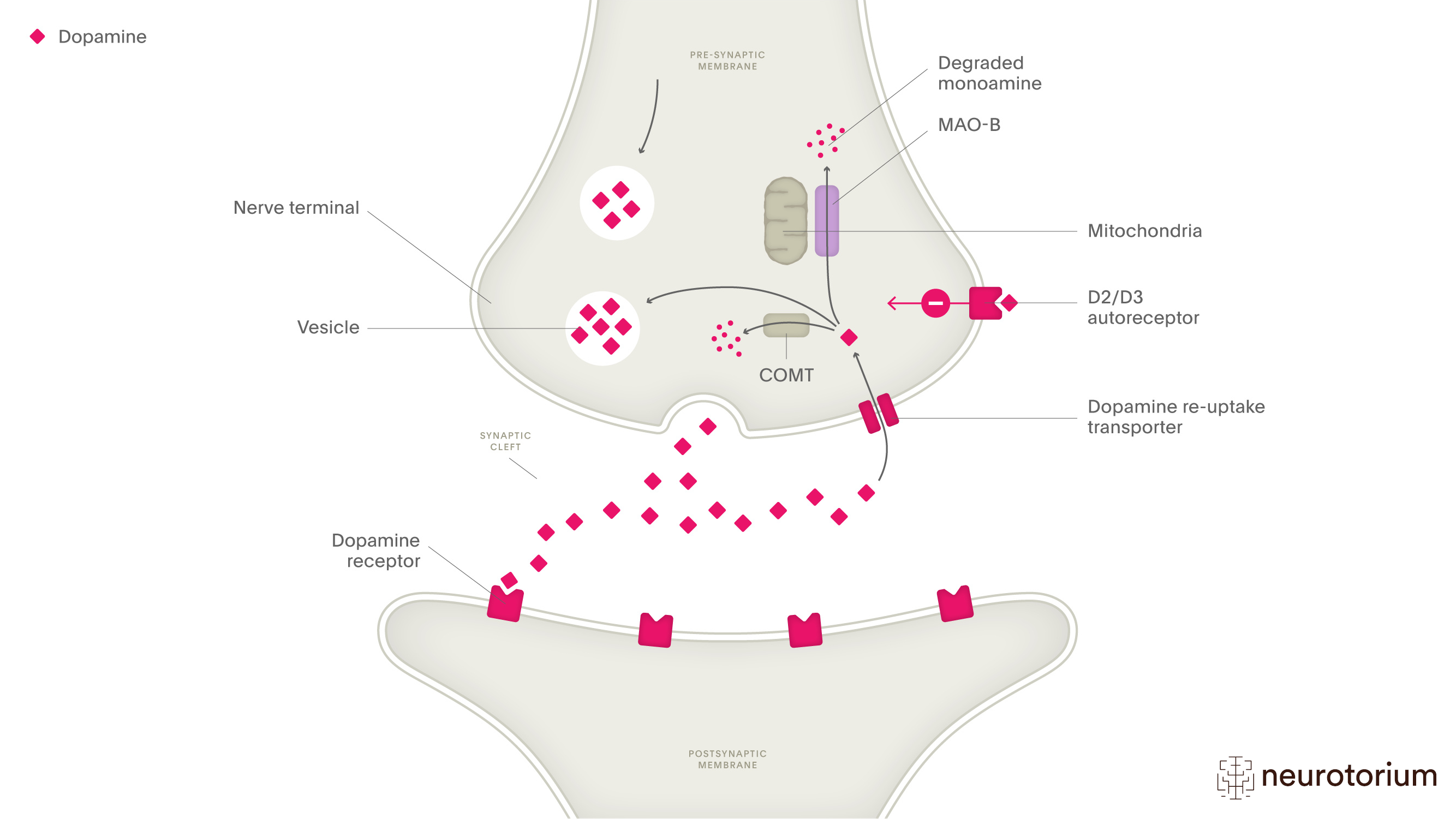
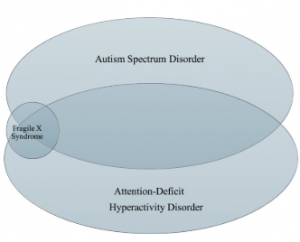
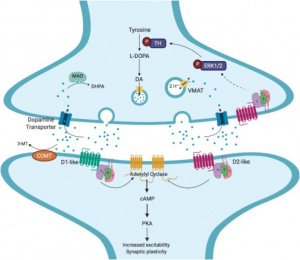
Often misunderstood as the brain’s “feel good” chemical, dopamine is a neurotransmitter that plays a crucial role in many bodily functions. Dopamine is essential for motivation and reward. It is released after completing something pleasurable like eating your favorite food, accomplishing a goal, or learning something new. Instead of making us “feel good” dopamine rather serves to reinforce these behaviors and motivates us to seek them out again. Dopamine is also essential for smooth and controlled movements, staying attentive and focused during tasks, and regulating mood[3]. So, what happens when dopamine doesn’t function the way it should? Dysregulation, or an imbalance of dopamine, can lead to symptoms like reduced motivation, mood swings, difficulty focusing, loss of reward, and movement disorders. It can also cause psychiatric and neurological disorders such as Parkinson’s disease, ADHD, depression, anxiety, and – you guessed it – autism spectrum disorder[4].
Piecing Together the Evidence: New Research on Dopamine Dysfunction in Autism
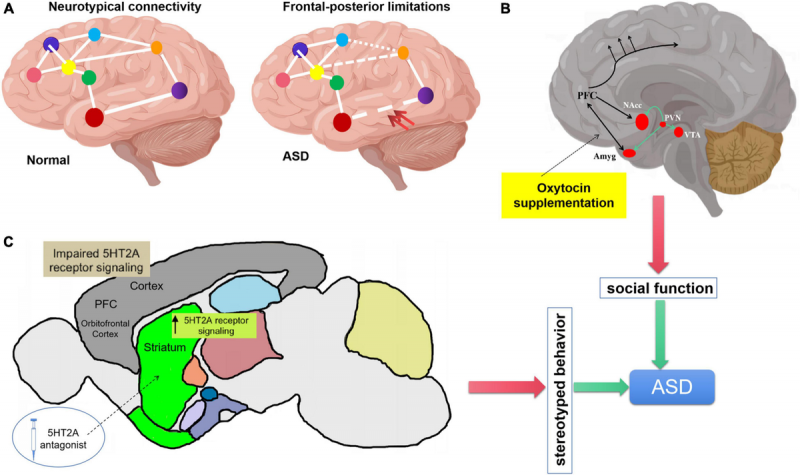
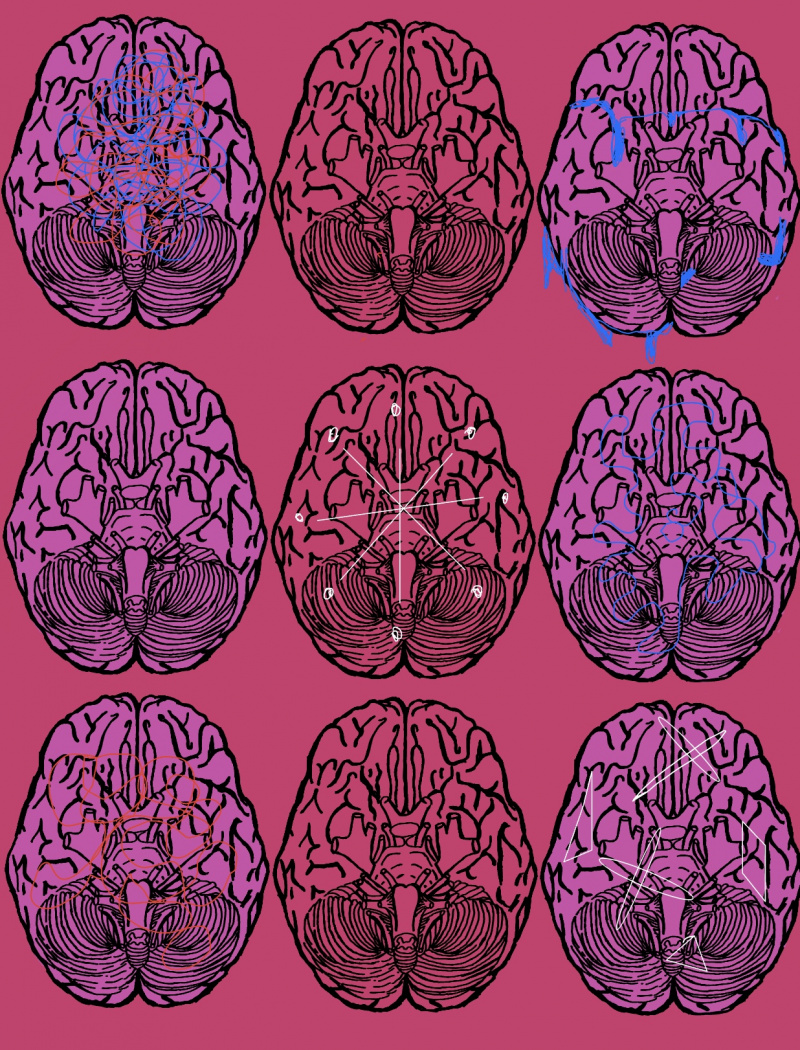
In the 2022 review article, “Modeling dopamine dysfunction in autism spectrum disorder: From invertebrates to vertebrates”, DiCarlo and Wallace argue that one possible subtype of ASD may be associated with dopamine dysfunction[5]. The article proposes that dopamine dysfunction could contribute to ASD by disrupting key neural circuits involved in reward processing, social behavior, and motor control. As mentioned earlier, dopamine regulates motivation, attention, and the ability to process social and environmental cues, all of which are impaired in ASD. Specifically, dysregulation of dopaminergic signaling in the striatum and prefrontal cortex (brain regions essential for reward learning and decision-making, rich in dopaminergic neurons) may underlie the social communication deficits and repetitive behavioral characteristics of ASD. For example, reduced dopamine activity in the medial prefrontal cortex has been observed in individuals with ASD, which could impair their ability to assign value to social interactions, leading to social withdrawal.

Additionally, abnormalities in dopamine transporter (DAT) function, such as altered dopamine reuptake or efflux, have been linked to hyperactivity and repetitive behaviors, which are common in ASD. Dopamine also modulates the balance between excitatory and inhibitory neurotransmission and helps to filter out neural “noise.” Disruptions in this balance are thought to contribute to the sensory sensitivities and neural hyperconnectivity seen in ASD. Finally, dopamine interacts with other neurotransmitter systems, such as glutamate and GABA, which are also implicated in ASD, suggesting that dopamine dysfunction may exacerbate broader neural circuit abnormalities[5]. Overall, dopamine dysregulation may play a central role in the neurobiological mechanisms underlying ASD.
The Missing Pieces
Dopamine dysfunction is undoubtedly an essential key to the puzzle of autism spectrum disorder, but many missing pieces remain regarding the exact mechanisms in which dopamine contributes to ASD. For example, it is still unknown whether dopamine abnormalities are a primary cause of ASD or a secondary effect of other genetic, neurobiological, or environmental factors[5]. The relationship between dopamine dysfunction and the heterogeneity of ASD is also not fully understood. Why do some individuals with ASD show hyperdopaminergic traits, such as hyperactivity, while others exhibit hypodopaminergic features, like social withdrawal? Finally, while some studies suggest that dopamine-targeted therapies may benefit certain individuals with ASD, it remains unknown how to identify which patients are most likely to respond to such treatments[5]. Addressing these gaps in knowledge is critical for developing more precise, dopamine-based treatments for ASD.
Solving the Puzzle
Dopamine dysfunction is implicated in autism spectrum disorder and is thought to contribute to symptoms like social deficits and repetitive behaviors, but the exact mechanisms remain poorly understood, therefore future research should focus on identifying biomarkers for dopamine-related ASD subtypes and developing targeted pharmacological therapies to improve outcomes for individuals with ASD. Hopefully, with these new discoveries and future research in this area, the pieces of the ASD puzzle will finally come together.
References
[1] CDC, “Data and Statistics on Autism Spectrum Disorder,” Autism Spectrum Disorder (ASD). Accessed: Mar. 19, 2025. [Online]. Available: https://www.cdc.gov/autism/data-research/index.html
[2] “Autism Spectrum Disorder – National Institute of Mental Health (NIMH).” Accessed: Mar. 19, 2025. [Online]. Available: https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd
[3] “Dopamine: The pathway to pleasure – Harvard Health.” Accessed: Mar. 19, 2025. [Online]. Available: https://www.health.harvard.edu/mind-and-mood/dopamine-the-pathway-to-pleasure
[4] H. Juárez Olguín, D. Calderón Guzmán, E. Hernández García, and G. Barragán Mejía, “The Role of Dopamine and Its Dysfunction as a Consequence of Oxidative Stress,” Oxid. Med. Cell. Longev., vol. 2016, p. 9730467, 2016, doi: 10.1155/2016/9730467.
[5] “Modeling dopamine dysfunction in autism spectrum disorder: From invertebrates to vertebrates – ScienceDirect.” Accessed: Mar. 20, 2025. [Online]. Available: https://www.sciencedirect.com/science/article/pii/S0149763421005650?via%3Dihub
[6] “Imaging-genetics of sex differences in ASD: distinct effects of OXTR variants on brain connectivity | Translational Psychiatry.” Accessed: Mar. 20, 2025. [Online]. Available: https://www.nature.com/articles/s41398-020-0750-9