The aging process is one we’ve studied as a people for as long we’ve existed. And extending our lives has always been a major motivation in those studies. Our current understanding of aging at a cellular basis is one of oxidative stress and mitochondrial damage. Over time, our cells create more and more reactive oxygen species (ROS) that cannot be broken down before doing their damage, which lead to the generation of more ROS. I’ll break down the concept and introduce a few interesting ideas from our class discussions.
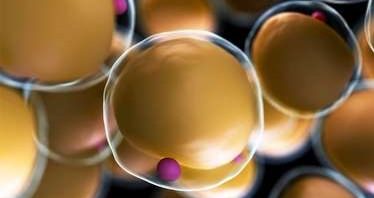
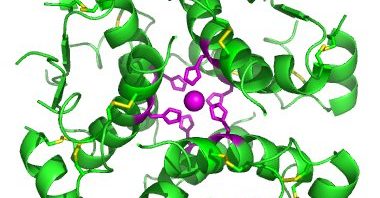
The mitochondria, the most well-known organelle in the cell. It gets its memorable nickname the “Powerhouse of the Cell” from its function, creating energy. The mitochondria can be thought of as a factory, but it can be better visualized as a furnace. Just like any bomb or engine, sugar breakdown is a combustion reaction. A carbohydrate reacts with oxygen and breaks down to water, carbon dioxide, and energy. So in the mitochondria, sugar is broken down and the heat/energy given off is utilized to generate energy molecules for the cell. However, this process isn’t perfect. Instead of becoming carbon dioxide, the oxygen molecules can be changed to reactive oxygen species, like superoxide.
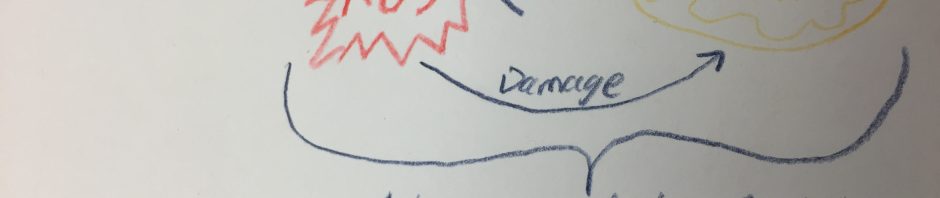
These ROS are dangerous, a given with the name reactive. They damage DNA, proteins, and membranes. The damaged DNA works less efficiently and increases the chances for mutations. The proteins that are damaged dysfunction and/or accumulate. Membrane damage along with protein damage are important for their impact on the mitochondria. The ROS generated by the mitochondria, turn around and cause it to generate even more ROS. This positive-feedback loop would lead to the accumulation of a lethal amount of ROS. Our body takes care of this with proteins that neutralize ROS. As stated above, ROS damage proteins as well. Over time, our body loses the fight against ROS generation. Leading to disease and aging.
How does this concept apply to us? Calories basically equate to energy for the mitochondria. Meaning that, calories, by virtue, lead to ROS as well. The oxidative stress of calorie consumption is a natural part of life and the aging process. Overnutrition exaggerates that stress. When our body takes in too many calories over a short or extended period of time, it generates more oxidative stress. How relevant is this to the aging process? That’s where we need to learn more.
There is interesting evidence in support of that. Rats have been shown to live longer if their amount of proteins neutralizing ROS are increased. That doesn’t hold true 100% of the time, though. Sometimes the opposite effect happens with similar proteins. The current hypothesis is that ROS are damaging, however, they do have a necessary function in the cell that can be disrupted. The most interesting idea I came across was that reducing caloric intake extended life span.
It has been shown in many experiments with varying mammals that reducing caloric intake by 30-50% below what the animals would eat if they had no restrictions, leads to a significant extension in lifespan. This idea is very interesting for thinking about extending life, but it’s also very applicable on the opposite side of the spectrum, overeating and reduced lifespan. Overeating is obviously a concern in many countries throughout the world and its effects on aging and possible controlling those effects calls for more investigation. Life-extenstion is also very interesting, but those studies called for reduced feeding during development. Reducing calories that far is hard to do in the first place, but its negative effects on even an adult’s body wouldn’t be worth any hopeful benefit in lifespan. Going forward, it will be interesting to see how the role of oxidative stress and overnutrition becomes a factor in preventing and treating illness.