By far this course has been one of my favorite at Concordia. I looked forward to going to Neurochemistry every day.
This course was a place where we could put our chemistry expertise to use and explore real world problems. It was so fun to have discussions surrounding real world science with fellow students and be able to apply our various backgrounds to the discussion.
Throughout the course we delved into various neural disorders that worked to incorporate the five goals of liberal learning Concordia has set forth as the cornerstone for capstone experiences.
Instilling a Love for Learning
Each week we explored a different neurological disease. Each week we worked to understand the science of the disease with each other through discussion Mondays and speed dating Wednesdays.
The love for learning was so easily instilled as we worked together to understand each piece of the puzzle. Not only was it immediately interesting to us all, but it was collaborative learning that made the class so exciting.

The atmosphere was full of students who cared about the subject material and were excited about learning all we could about the disease and the best ways to treat and/or cure it.
The exciting real life learning we did in neurochemistry instilled in us a passion for learning and discussing the things we learned with one another, and also to share what we had learned with the larger population through our blogging.
Developing Skills and Transferable Intellectual Capacities
What made this course so great was the ways in which it was applicable to daily life. We all had heard of the diseases we discussed, and had an interest in figuring out what chemically was causing the diseases.
By having these vested interests, it was easy to study the diseases in depth and then use the knowledge we acquired to write blogs to share the information with the broader community.
Blogging was one of my favorite parts of this course. It was a chance to put the complexities of chemistry we had researched throughout the week into an understandable story for people outside of the Cobber Chemistry Bubble to engage.

The skills we developed will be so useful in our professional careers as we are required to explain complex science to people who have a various array of scientific literacy.
As a physician in particular, I find the skills I have developed in this course to be essential to relating to patients and making them feel comfortable in their health journeys.
Developing Diversity of Disciplines
Our class had a wide array of expertise. Many of us were chemistry majors, but we also had several biology majors and psychology majors. This variety aided in our collaborative learning immensely.
I have very little understanding of psychology, and very little interest in it. By those who live and breathe psychology were so helpful to me.
They were the ones who understood the papers about schizophrenia, bulimia nervosa, and autism best. They were the ones who could explain where clinical treatments currently lie, and speak from experience in working with individuals who suffer from these diseases.
In this way, the course has instilled in me the importance of interdisciplinary work, and the invaluable resource that is new perspectives.
It is always humbling to be around someone who’s strengths differ from your own. I was blown away by the different perspectives in this class and how they shed light to the problems we were discussing. They helped me to understand the diseases and solutions in new and deeper ways.
The interdisciplinary work in this course helped me to understand my own abilities and where they are helpful as well as where they fall short in looking at health concerns. I will carry this awareness and value with me as I venture into the world of medicine.
Cultivating Holistic Self-understanding
As I have already touched on, the interdisciplinary work we did in this course helped me to understand how my training in chemistry has both prepared me, and in some ways hindered me in my abilities to solve problems.
With a chemistry brain I am very good at deduction and problem solving, but terrible at memorizing specific bits of information for each disease. In this way, I relied heavily on my biology and psychology classmates to fill in the missing pieces.
It was also through this course and collaborative learning that I became aware of my great training in taking lots of information and organizing it into a helpful and useful format.
Inspiring BREW

As an aspiring physician I found this class to be so applicable to my future career in medicine. I found the ways of discussing both the science and the societal norms surrounding each disease we looked into to be asking the deep questions of what this information means to the world.
From this experience I have gained the ability to critically engage scientific research and the ways in which understanding the deep chemistry of the problems can help in developing treatments and prescribing medicines.
As a chemistry major, graduating from Concordia College in just four short days, I feel so prepared to be a thoughtful and informed responsibly engaged participant in the medical profession, both locally and globally. Both this course and all those I have taken at Concordia have prepared me so well for the future ahead.
The Autism Diet…Is It Real?
What is Autism?
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder that is characterized by impaired social interaction. Other symptoms include restricted repetitive behaviors, interests and activities. These symptoms often lead to impairment in social and occupational functioning. The cause of ASD is still not completely understood, however a recent review article summed up much of what we know so far about the pathology of ASD. This article essentially tells us that there are a number of genes that are linked to ASD a number of them code for proteins that impact the growth and development of neurons and synapses. One way I like to think of what is going on with the neurons is that they are not communicating very well. Now the brain has multiple regions to it that each has a specific function and for each of these brain regions to work properly it must be connected to other parts of the brain. One symptom we see in ASD is over-connectivity of neurons within a certain region but under-connectivity between the brain regions. Because ASD is a spectrum we see a wide array of symptoms and a wide array of severity of those functions.
Is there a diet suggested for people with ASD?
Many parents of children with ASD report that their child’s behavior improves when they eat a dairy and gluten free diet.
Does this diet actually work?
In 2009 a review of research concluded that there was not enough evidence to say empirically that a gluten and dairy free diet helped with autistic behaviors. However there has been more recent research into the topic and two different studies (One from Denmark and one from Penn state) both showed that if the diet was stuck to very strictly for at least 6 months or more, patients showed improvements in behavior. Improvements meaning less hyperactivity, temper tantrums and speech skills.
How hard is the diet to implement?
It can be difficult to very strictly watch the diet of any child and perhaps especially one with autism so the Autism Research Institute issued a couple helpful tips to parents about implementing this diet. The full article can be found here. But to sum up they essentially said that taking “cheat” days can be a bad idea and to really watch out for foods that could be hiding gluten or dairy.
A Capstone Experience
The main goals of liberal learning include the development of a love for learning along with a deep understanding of how what you learn can impact both interdisciplinary and intradisciplinary understanding. These goals are meant to enable students to draw connections across academic boundaries while promoting connections to the world outside academia to enrich the lives of those who our knowledge might help. In my four years at Concordia College, I have never experienced a class more suited to these goals than Neurochemistry.
At first glance, Neurochemistry appears to be yet another science course offered at Concordia. With an emphasis on developing an understanding of remarkably complex neural pathways involved in neurological diseases, Neurochemistry explores the brain’s circuitry to better understand how these diseases are developed and how they might eventually be cured.
However, there is something that sets this course apart from many other courses offered at Concordia. While a goal of the class is to delve into the world of neurochemisty and all of its complexities, there is another purpose beyond simple content mastery. After learning the ins and outs of the science behind a particular disease, a discussion is opened as to how this new understanding can impact the world outside of neurochemistry. The focus is not to sequester the information we understand within the scientific community, but to share and spread what we have learned with the public at large to foster a better understanding of what we have learned.
Between blog posts, public service announcements, and cross-disciplinary discussions, this course has showed me the importance of widening the base of impact that scientific discoveries can have. Too often, novel scientific discoveries are limited to a highly devoted scientific population without much consideration for how the public at large could understand what has been discovered. A goal of this course was to distill that information into a form that makes available the impact of current research and discuss how these findings could lead to changes for the better in the lives of people.
The motto I’ve heard consistently at Concordia is an importance to BREW, or become responsibly engaged in the world. Neurochemistry has shown me both what is currently lacking and what could result from a scientific community more in tune with responsible engagement in the world.
The Impact of Neurochemistry: My Capstone Experience
Around March of 2015, I was constantly emailing the professor for the Neurochemistry class, trying to get registered. The class was already full, and I was pretty bummed. I thought that this class would allow me to learn more about how the molecular signaling cascades in the brain attribute to how we behave and function as humans.
Now, as I am taking this class a year later, I realize that I was completely wrong; this class taught me much more than that.
I know that that sounds cliché, but it’s true. I went in to this capstone class expecting to just learn more about the brain. As it turns out, I learned more about how we can contribute to society with the knowledge we have, what the current issues are involving neuroscience (i.e. autism, schizophrenia, obesity), and how I am capable of much more than I had thought.
This was one of the first classes that I retained most information from the class AFTER the last day. I also enjoyed GOING to class. I never felt that pain and suffering that most students feel as they trudge their way to class on Mondays.
I looked forward to tackling the scientific articles we read (mostly because I didn’t know what half the words meant on most of them, so I was excited to hear some explanations). The articles were very interesting to read because they were topics that pertained to today’s society.
They weren’t articles that I usually read for classes. They talked about real issues, current science, and the implications of future research. This kept me interested and fascinated throughout the course.
Another aspect of the class that we get to take home with us was how we, as Concordia Neuroscientists, can contribute to society utilizing our knowledge and understanding of the topics that we discussed. We had a diverse class, with some people wanting to go into entomology and some wanting to go into clinical psychology (Hint: The last example was me).
Now that I’ve talked about how awesome the class was and how I can take what I learned and use it to Become Responsibly Engaged in the World, I also wanted to reflect on my emotional experience throughout this class.
That sounds a little lame, but hey, I’m a Psychology major. Emotions were bound to come up.
I was actually really nervous for this class. I haven’t had a lot of chemistry background, and so I knew that I would have to work really hard in this class. I knew that I would be behind my peers, so I was definitely not very confident at the beginning of this course.
Once the course started going, I started to feel more comfortable. I was able to answer questions that some other people weren’t able to, and I was able to utilize my psychology background when talking about things such as Bulimia Nervosa and Schizophrenia. Being able to answer questions like that also had made me realize that I do retain a lot more than I think I do, and that I am a lot more capable than I think I am regarding science.
My knowledge and confidence grew in this class almost exponentially. In fact, I am leaning more towards research as a potential career path. If you would have told me that about a year ago, I would have laughed in disbelief. I loathed research, research articles, basically anything that had to do with research.
That was until our first Neurochem exam.
The paper that we had to read for our exam was about Alzheimer’s and the over-phosphorylation of eukaryotic initiation factor 2-α (eIF2-α). Basically, protein expression doesn’t work properly, and signals are sent throughout the cell to promote cell death.
On one of the last pages of the paper, it stated that this eIF2-α was not only found in Alzheimer’s and Type II Diabetes; it was also over phosphorylated in Autism Spectrum Disorder.
If you know me or have taken any class with me, you would know that this stood out like a sore thumb to me. I am extremely fascinated by ASD, but I have only focused on the behavioral aspects of the disorder. Working as a Behavior Therapist, that is mostly all that I do.
However, learning about eIF2-α phosphorylation inspired my project for Neurobiology, which then inspired my research proposal for Neuro Senior Seminar. And now, I can proudly say that I am strongly considering a career path in neurological research regarding Autism Spectrum Disorder.
In class, we also read a paper about the potential causes for ASD. The schematic from the paper below shows how simple it is:

Pretty easy, right???
Looking at this schematic and breaking it down inspired me. I would love to spend my career trying to tackle at least one of the malfunctioning proteins or transcription factors and, potentially, discovering more about ASD.
The whole point of my little soap box was to mention how much Neurochemistry has impacted me. I am very thankful for this class, and I encourage anyone to take it for the capstone experience. I know that because of the knowledge that I have obtained through this class, I will be able to go out into society with more empathy, more confidence, and more inspiration.
Neurochemistry: A Capstone Reflection
Neurochemistry, or neurochem as we like to call it, has been single handedly the most interesting class I have ever taken. Neurochem has spiked my interest in numerous areas of study and educated me to a whole new level on various subjects. I have thoroughly enjoyed nearly all class periods and learned so much more than I initially thought I would. This class was the pinnacle of my chemistry major and neuroscience minor during my college career and I know that because of this class I will follow many of these topics as they become further researched. This class is the reason I have chosen neurodegenerative disease research as a possible career plan for myself.
In this class we delved into the most recent research on hot topics for diseases and disorders. We broke down what each main article had to say, answered any questions we had by doing research of our own , then had a class discussion on the big picture of the problems and what maybe we can do as scientists to help get closer to answers we don’t have. This class helped us as students understand what it means to learn in a liberal arts school and how we can help change the world.
The first goal for a liberal arts education was to instill a love for learning. In this class we learned about the most recent research there is and I found that fascinating. I love that I not only can understand the problem, but also what needs to be done to fix it and even give input of my own. Very rarely do I have classes that I actually enjoy going to, however, this class made me feel like I can make a difference and actually led me to decide on a possible career path.

The second goal is develop foundational skills and transferable intellectual capacities. In this class we first started out talking about a lot of basics that we need to know to understand the articles. Most of the information was not new to me for I have a background in neuroscience, however, it gave us a foundation needed to move on to bigger topics. We also read many scientific articles which, a less obviously, helps us understand scientific literature and will help us in the future when writing and reading may be essential to our careers.
The third goal of a liberal arts education is develop an understanding of disciplinary, interdisciplinary and intercultural perspectives and their connections. In neurochem we read about many different diseases, disorders, and conditions. It helped us understand that the brain is a very plastic organ and is extremely complex and fragile. We learned that when one area goes wrong it can trigger a number of different problems. Many diseases and disorders in the CNS are different, but in many ways they are all connected. This class challenged us to see these differences and similarities and explain why they might be. Much of the class was coming up with hypotheses as to why something might be happening the way it is.
The fourth goal is cultivate an examined cultural, ethical, physical and spiritual self-understanding. In this class we saw many different ways the human mind works. Using the knowledge we gained from the readings we are able to examine ourselves and maybe answer questions as to why we think a certain way or why we act a certain way. There is a lot we can learn about human behavior from observing the effects of diseases and disorders. This class helped us be able to execute many of these actions.
Finally, the last (but certainly not least) goal of a liberal arts education is to encourage responsible participation in the world. As I stated before, this class has spiked my interest on many topics and I have become quite passionate about many over the past few months. It has changed the way I think about food. It has changed the way I look at someone when they are acting out of the ordinary. It has even changed the way I think about certain topics like alcohol and marijuana. I have told many people what I have learned from the class and what they should know to live a smarter and healthier life. This class makes me want to research certain diseases because I really think I can help research in the field. One of the best classes I have ever taken.
Image citations:
https://i.ytimg.com/vi/aHp2hkue8RQ/maxresdefault.jpg
https://www.google.com/search?q=neurochemistry&source=lnms&tbm=isch&sa=X&ved=0ahUKEwj-9PKqqq_MAhWEND4KHV_7COAQ_AUICSgD&biw=1920&bih=929#q=neurochemistry+lab+work&tbm=isch&tbs=sur:fmc&imgrc=398aPFItkEwGgM%3A
Autism Spectrum Disorder
Autism spectrum disorder is commonly known for its social impairment, and the symptoms include abnormal social interaction and communication, and stereotyped behaviors with restricted interest. The neural mechanisms responsible for these behavioral symptoms have been intensively investigated by the scientific community in the last 30 years.
Researchers genetically modify rodents in order to better understand how Autism affects the brain. The genetic mutations produce a range of symptoms similar with the symptoms found in humans, but how the genetic mutations lead to behavioral symptoms of Autism is not fully understood.
Between the potential mechanisms underlying Autism are: neuroanatomical abnormalities, and excitatory and inhibitory imbalance. How these mechanisms are related, and how they give rise to autism is still being investigated.
Neuroanatomical abnormalities result from abnormalities in brain development, that can be caused by gene mutations, inappropriate levels of neurotrophines (a family of proteins that induce the survival, development, and function of neurons. They belong to a class of growth factors, secreted proteins that are capable of signaling particular cells to survive, differentiate, or grow), and environmental factors which, together or independently, are affecting brain development and leading to pathological states.
The brain can have excitatory and inhibitory synapses, that together, work in a balance that maintain our normal functioning, filtering main information and inhibiting “noisy” information. To maintain such balance, many proteins and neurotransmitters work together. In autism, the brain displays local over-connectivity and long range or inter-regional under-connectivity, both caused by excitatory and inhibitory imbalance. The imbalance is mainly caused by a flaw in one or more of the proteins responsible for maintaining the proper functioning of synapses. The defects in the proteins can be a result of gene mutations and environmental factors.
.
The causes that lead to the onset of autism are still not fully understood, but with the scientific advancement, researchers are getting close to understand how the autistic brain is being affected by gene mutations and how we could target specific proteins in order to treat the disorder.
What causes Autism?
Autism had dramatically grown in the past fifty years. The US documented that 19 out of 10,000 individuals had autism in 1992. This rose to 1 in 150 in 2002, followed by 1 in 110 in 2006. As it can be seen, the growth in individuals with autism is huge. The reasons why this number has increased so greatly is not well known. One known contributor is the expansion of the autism spectrum, but there has to be more to it. Some people think vaccines are the cause, and others think genetics or even stress. So with the great confusion, my class decided to look deeper into autism and tried to define the true cause of it.
After reading and analyzing our paper for the week, some potential areas were targeted for a likely cause of autism.
As a whole, we discovered that very simplistically, neurally there is too much glutamate, excitatory neurotransmitters, and not enough GABA, inhibitory neurotransmitters, in the brain. This is causing a myriad of problems. Generically abnormal neuron migration and synchronization is occurring.
Looking deeper into the actual signaling pathway, there are numerous problems that could be occurring. One of which is too much protein synthesis, which produces more than necessary mRNA through over activity of FMRP and eIF4E. Another area of concern is the miscommunication between receptors NRX and NLGN, which cannot dimerize properly and is causing the imbalance of excitatory and inhibitory neurotransmitters. SynGAP also can be a part of potentially causing autism by not being shut down because it assists in the production of protein. In individuals with autism, they also see a decreased amount of Reelin and dysfunctions with Shank. The image of the pathways is located in the paper on top of page nine.
As you can see, there are various problems that can occur with autism and there is not one specific area that has been discovered to cause it.
I was specifically interested in environmental factors that could induce or cause autism. From what I found, there is not one environmental factor that causes autism, but rather, there are many different items that can induce autism in individuals with a genetic predisposition.
Some of the factors I found were diet, heavy metals, pesticides, stress during birth, drugs, and medications. Vaccines are a factor many individuals believe is the cause for autism. In many recent findings, each of them said that vaccines do not cause autism and it is much safer to vaccinate children from deadly illnesses than to have fear that they could get autism.
Again, there is not one distinct reason for the cause of autism, but tons of research is being done to see if it can be narrowed down to a specific area of the brain or an environmental factor in order to prevent autism growth in the future.
Why Are We Only Treating Half of Autism?
In the United States today, approximately 1 in 68 children are diagnosed with Autism Spectrum Disorder (ASD). ASD is a disorder of the brain that can include, but is not limited to, social interaction difficulties, communication challenges, and a tendency to engage in repetitive behaviors. Autism is often misunderstood both in the public and in the scientific community. A large part of the problem is that it is not understood in the brain.
Autism diagnosed on a very large spectrum and people with the disorder vary on levels of functionality and ability to do things such as communicate, socialize, and control their behaviors. As for genetic factors, there are diverse variations underlying the development of ASD and this limits the development of medication for people living with ASD. Currently, there are only a few FDA-approved medications for ASD including a drug called Risperidone. Risperidone is a dopamine antagonist that acts as an antipsychotic in the brain and is most commonly used to treat schizophrenia and bipolar disorder. The problem with using this medication in ASD is that it doesn’t help with all the symptoms of the disorder. While taking the antipsychotic, there is a reduction in hyperactivity, irritability, and repetitive behaviors that people with ASD tend to experience. When these symptoms are treated, there still are the problems with social withdrawal and communication skills.
With this limited treatment option, the focus in research lies on cause of the social and communication impairments. Likely, the “core” of ASD symptoms can be attributed to problems in excitatory synapse transmission. As the brain was developing in ASD children, The greater the malfunction of excitatory pathways in the brain, the greater deficits. In excitatory pathways of ASD patients, studies have shown that there is improper development in adhesion molecules and scaffolding proteins. When these components are incorrectly developed, the excitatory pathways associated with social skills and communication are impacted negatively.
Unfortunately for ASD patients, the misunderstanding of this pathway malfunction is the reason they cannot be effectively treated. For this disorder, medication may or may not be the answer, but without understand the neuronal pathways affected, the scientific community can never find out. It is possible that behavioral therapy may be the most promising way to treat children with ASD. As research on autistic brains continues, hopefully the thousands of children with the disorder can benefit. Regardless of research outcomes, children with autism are full of light and deserve to be advocated for in any way possible. Advocacy needs to happen in the scientific, medical, and public settings for the 1 in 68 children currently living with ASD.
Fun fact: April is Autism Awareness Month!
Oxytocin is More than Just a Love Hormone: Could it be the Future for ASD?
It isn’t really possible to narrow autism down to one specific difference or symptom, really it is a combination of many different things. Every single case is unique, which is what makes it so difficult to treat.
In the 70s/80s it was estimated that 1 in every 2,000 kids had autism, the current numbers are 1 in every 150 8 year olds are diagnosed with an autism spectrum disorder (ASD). ASD would include subcategories such as Aspergers and pervasive development disorder. Since autism has been more recognized and diagnosed there was an initial spike in the number of cases, but even now with a pretty standard diagnosis there is gradual rise in ASD cases.
The common denominator of autism symptoms is misfiring of normal neuronal synapses. Many proteins, hormones, and genes that play a role in synapse are not working correctly in autism. It is difficult for them to connect longer synapses and shorter synapses tend to over fire
This is where the overstimulation comes into play. Because there is so much firing going on in one place it is difficult to connect the other synapses correctly. Many autistic people have a sensitivity to outside stimulants such as lights, sound, and movements.
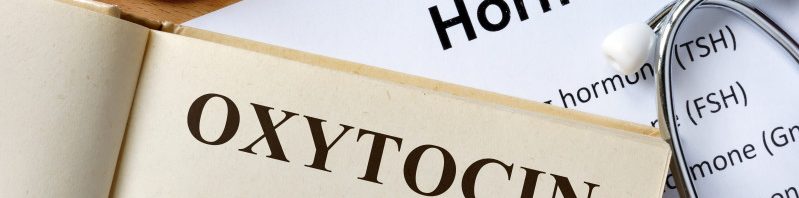
They also have difficulty handling social situations and other people’s emotions. It is found that autistic people have lower levels of oxytocin. Oxytocin is known as the “love” hormone. It is produced during sex, childbirth, and breast feeding. During the first 6 months of a relationship there are elevated levels of oxytocin, this is the honeymoon stage.
Its emotional responses include trust, relaxation, and psychological stability. In response to stress oxytocin acts as an anxiolytic. People with higher levels of oxytocin are more extroverted and are more sensitive to other people’s emotions.
A small study was done on volunteers with mild ASD where they used oxytocin as a treatment. The oxytocin was taken as a nasal spray. The individuals were better able to handle social situations both at home, in public, and in a clinical setting.
After the success of that study they were given a grant to continue this research. Is this the new future for autistic people? Will they be able to change the social behavior of autistic people? How available will it be? Where do we draw the line, will people take oxytocin just to be more extroverted? Should everyone be more extroverted? With more research, who knows where this will lead us.
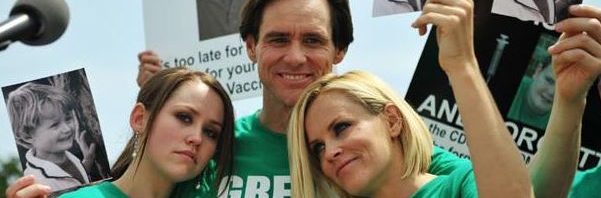
Who Done It? When Vaccines Plead Not Guilty to Being the Source of Autism
Autism is on the rise in the United States. The prevalence has increased from 1 in 110 in 2006 to 1 in 68 in 2010. This increase has led to more awareness surrounding the disease, as well as increased hype and concern.
Jenny McCarthy’s infamous campaign against vaccines as the culprit of her child’s autism has gained a lot of attention, and caused a “red scare” on vaccines.
This campaign, however, has been more detrimental to the health of the country than good. Outbreaks of diseases not seen since their vaccine development have caused detrimental consequences to children whose parent’s decided against vaccination.
Vaccines no longer contain the mercury that once was thought to cause autism—but the rate of autism diagnoses still increases. Thus, vaccines are not the culprit—the CDC confirms this. This then begs the question, what is?
Who Done It? Will We Ever Know?

(Won, H., Mah, W., Kim, E., 2013)
As one can observe from this lovely figure taken from this week’s research paper—the culprit lies in a mess of chemical signaling pathways. Not only can we not pinpoint exactly which red blob—the red are highlighted to signify that they are known to malfunction in autistic individuals—is responsible for autism, but this diagram doesn’t even account for all the variables.
There are considerations that need to be done about where in the brain the problem is occurring. The science points to the cerebellum and specifically in the Purkinje cells. However, there are also major differences that occur in autistic brains in various other structures—such as the hippocampus, corpus callosum, and amygdala.
Along with this, there are also environmental factors at play. There is a high metal sensibility in autistic brains—that cannot be traced to vaccines—but must be traced to something.
There are also neonatal concerns. Infection during pregnancy increases the risk of autism development in the child.
With all of these factors, the solution to the crime may never be solved.
What do we Now? The Evidence is Mounting.
Throughout the week we each investigated one of the red blobs. It seems that each plays a significant role in the development of autism, but each plays a different role that connects to other pathways, diseases, and complications.
Some of the more promising leads are pointing to Purkinje cell development in the cerebellum. These cells seem to over develop in the signal receiving end of the neuron—called the dendrite—while under developing in the signal sending regions—the axon.
(photo of Purkinje cell)
This results in loss of correct connections being made. The red blobs likely involved—that are likely to be caught “red handed”—are the neurexin and neurolignin connective proteins as well as the REK protein thought to guide axonal growth.
More evidence points to these culprits as the cerebellum’s functions are discovered. More and more, there are discoveries that link this stereotypical motor center with behavioral and social actions. If this is the case, the cerebellum and its Purkinje cells could be the eyewitnesses needed to point to the autism instigating culprit.
What will the penalty be? Treatment of ASD.
The culprit is on the verge of being caught. While the chemistry and brain functioning is complex, the story is continuously being uncovered. This leaves us with the judicial duty of questioning, what will we do once the culprit is identified?
We need to think critically about what autism is and what it is that is harmful about it. Yes, some behaviors that result from the disease are extremely harmful, and there is a lot to be said about the benefits of improving treatments.
However, there is a question about “odd” behavior and “bad” social skills. Should everyone be the same and have the same ability to interact? What is wrong with someone who doesn’t like to interact with others as much as they like to study art or science, for example?
By uncovering all there is to uncover about autism in the brain we run the risk of discovering what makes certain personalities develop over others. And this is a slippery slope.
Thus, this quest for who done it is one of pointing fingers instead of solving true problems. The autism scare must stop being about the hype, and start being about the science to treat the harmful aspects, while leaving room for individuality.