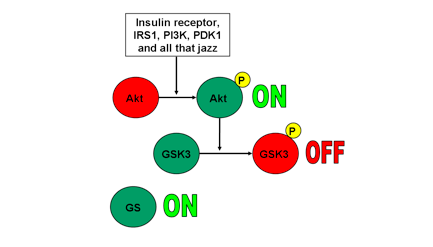
This week in class, we discussed the Akt-GSK3 pathway. The obscure name is enough to make most readers click on or scroll down, but before you do, I recommend you read just a little bit further. This pathway affects many aspects of your life and probably plays a role in a condition affecting someone in you know or maybe even you personally. The following list provides some examples of conditions associated with the Akt-GSK3 pathway:
- Addiction
- Parkinson’s Disease
- Schizophrenia
- Bipolar Disorder
- Depression
It’s incredible that one pathway can be implicated in and targeted for treatment for so many problems. Research into this pathway can lead to many important findings, improving the lives of many people in the process.
Research on the Akt-GSK3 pathway began when scientists found lithium to be an effective treatment for bipolar disorder. Lithium acts to disrupt GSK3 signaling inside the cell. Inhibiting of GSK3 activity has a variety of effects in the brain. Among them is the inhibition of serotonin-inhibiting receptors. Serotonin levels are often decreased in major depressive disorder. Antidepressants (specifically a class called SSRIs) act to increase the levels of serotonin in the brain. Inhibiting GSK3 has a similar effect to these SSRIs; therefore, lithium acts to decrease the lowness of the down periods in bipolar disorder. More selective GSK3 inhibitors are also being developed as depression treatments.
In schizophrenia, many atypical antipsychotics exist, but nearly all of them have the ability to act on the same class of receptors called D2-receptors. While it was thought this was the primary means of affecting psychotic behavior, it has been shown that other pathways are affected by these drugs. It is unknown whether the initial affected pathway, the newly-discovered affected pathways, or a mix of both cause the effects of antipsychotics. With further research, it may be possible to isolate a more specific target, producing more efficacious treatments with fewer side effects.
In Parkinson’s, the Akt-GSK3 pathway may contribute to brain cell degeneration, though the mechanism for this is unknown. Researchers discovered this link by examining the cellular effects of the neurotoxins used to create Parkinson’s-model rats in the laboratory. Further research into this pathway could be used both to treat and hopefully prevent or delay the onset of Parkinson’s disease.
Dopamine has been known to be an active part in the physiology of addiction. All reinforcing stimuli facilitate the release of dopamine in a certain part of the brain. Dopamine also acts on D2-receptors which, as stated previously, affect the GSK3 pathway. It is unknown whether addictive substances exert their effects through the Akt-GSK3 pathway or whether activation of this pathway from additional dopamine is merely an additional effect. It may be worth examining this to see if addiction can be curbed or even prevented in the future.
One other important thought we examined in our discussion is development of these new pharmaceuticals. It is important for them to be specific enough so as to avoid side effects, but also broad enough to address enough symptoms as they can. Also, a drug must be able to get to its target, which further complicates the process for researchers. Modern medicine is capable of many things, but innovation takes time and money. The human body also creates obstacles because not every drug can make its way into the brain or can be absorbed fast enough to provide relief. These concerns must be addressed when designing drugs.
Those are the facts we currently know. Facts, however, should bring questions to mind. We, as consumers and patients, must also ask ourselves the following questions: What separates “normal” from disorder-related behavior? What separates personality from irregularity? Is the behavior we see a result of something we can change by adjusting our lifestyle (e.g. exercising, maintaining a regular sleep schedule, eating healthier, lowering caffeine consumption, etc.) or is it the product of a genetic anomaly that would ideally be treated with medication?
Medical innovations are wonderful, but consumers must make decisions regarding what they put in their body based on their own NEED. Pharmaceuticals are not living beings that know to just go one place or only do one thing; they are chemicals designed to act on the body, many times to correct an imbalance. They act all over the body, not just in one place (though the action in one place produces the desired effect). The human body maintains a functional balance, each part affecting the whole. Putting one chemical in the brain affects one part of the balance, but because we cannot stop a chemical from circulating throughout the body, the chemical will act on other cells, causing additional effects. If we can naturally, through a lifestyle adjustment, correct an imbalance to alleviate symptoms while improving other bodily systems, it is clearly the better option because it usually does not produce negative side effects (except for less free time due to exercise, more sleep, preparing healthy food, etc.). Some problems arise from a lifestyle choice, but others are the result of things that are out of one’s control. This is where pharmaceuticals should find their niche. We have the ability to develop amazingly efficient drugs to help those in need, which is why research to help these people should continue. We must also be hesitant to attribute conditions to individual choices, but must also be careful not to immediately jump to the conclusion that pharmaceuticals are the best option. Natural remedies can alleviate symptoms and improve overall quality of life, but their maximum effect has a limit; drugs can treat the specific symptoms we need them to, but can cause side effects because of the need to get to the target area and the need to address certain symptoms. Patients acting as consumers and medical professionals acting as distributors must find a balance between the two to produce the best results for each patient.