Here I am again, writing about food, obesity, and the brain. This article really was about obesity though, and it’s not that surprising that when there has been an connection to weight I have taken the opportunity to write about it in my blog, because like so many Americans I feel like I am constantly thinking about food. The central role of food in our society is undeniable. Holidays, dates, life in general is planned around food. How to get closer to your kids? Eat dinner with them. Food is often used as a reward for good deeds, good grades, even potty training.

Why is this such a big deal? Well, there are a couple of different parts of the brain that are particularly associated with food: the part that tells you when you are hungry or full, and the part that feels the reward, how good a food tastes, etc. Leptin and insulin have been found to play a crucial role in the first part, maintaining food intake homeostasis, making sure that the body receives the appropriate nutrients, and maintaining energy expenditure. At the most basic level, how this works is that leptin and insulin work on the NPY/AGRP and POMC neurons. When there are decreased levels of insulin and leptin it stimulates the NPY/AGRP neuron which in turn stimulates food intake. Decreased levels of insulin and leptin stimulate the POMC neurons, giving your brain the signal that your body is full. Neat stuff, really!
When you enjoy eating food is stimulates the dopaminergic neurons which are associated with reward. This can become a learned behavior when food is used as a reinforcement for a good, or a positive reinforcement which would imply that the consequence increases the frequency of a behavior or maintains the frequency. A child who is rewarded with candy for finishing their homework may get to later years in their education and find that they want candy to do any homework at all. There have been studies that think that food reinforcement may be important to obesity studies (http://www.ncbi.nlm.nih.gov/pubmed/17907820). Food reinforcement for one good behavior may turn into reinforcement for multiple behaviors and turn into eating often, even when not hungry. Does anyone else ever feel like they can reward themselves for a good workout by eating something they know they shouldn’t eat, like a second piece of cake, or go out to eat for no good reason when you have plenty of delicious things to eat in the fridge? That is an example of learned behavior and using food as a positive reinforcement. So is this a part of what is leading to obesity in America, overeating, emotional eating? Just a few thoughts.
Partying, Partying, Yeah!
In the United States, there is a large use of alcohol among adolescents and college students. This could be influenced by TV shows such as Jersey Shore or rappers such as Lil Jon and his song “Shots”. These images have been shown to adolescents and now there has been an increase in alcohol use nationwide. Along with this increased substance abuse, there is also an increased rate of alcoholism. This increased rate of alcohol use gets the chemist inside me giddy at the idea of learning exactly how alcohol acts on the body and how we can use that information to help the problem.
As it turns out, there isn’t an “easy” explanation on how alcohol works in the body. There are several receptors on which it acts in the body, the most important of these receptors being NMDA and GABA. NMDA function is inhibited and GABA function is increased both of which can be attributed to the cognitive impairment effect of alcohol. After the initial stimulation of these receptors, there is a “second wave” of signal transduction involving opioids and endocannabinoids which play a role in the development of an addiction to alcohol. These two waves are the big important ideas when it comes alcohol acting on the brain.
As far as our substance abuse problem in the United States, there needs to be a solution to it. Personally, I think that there are two main things we can change that would help the problem. The first step would be to lower the drinking age. I feel that this would help in a couple ways. First of all, I feel that this would ease people into the idea of alcohol in a safe controlled environment. Generally, the first time an individual is exposed to alcohol would be at a party either in high school or college and they wouldn’t know what to expect or when they should stop compared to if we lowered the age, they could wait until they had their first drink in a controlled environment with their parents who could help them through it. I also feel that this would eliminate some of the mystical aspect of alcohol as we wouldn’t want to go behind our parents back to see what it was like but rather just drink it in a controlled environment and be more relaxed about it. The second thing I think we could easily change is the portrayal of alcohol in mass media. Like I stated before, there is a huge “party” aspect to modern music and TV shows. I feel that if we eliminate this, adolescents would be less likely to act like their idols and not go out drinking for drinking sake. These two things, although probably wouldn’t eliminate alcoholism in the United States, would most likely help control it.
Concussions and Checking in Hockey
We have all heard of concussions. Someone hits their head and in our culture generally we think or tell people to “shake it off”, but is that really a good idea? As a player, I know the temptation to get back on the field and make things happen. We all have seen professional players return from head injuries in a matter of days. There has been a lot of hype in the media about the dangers of concussions, but I for one, while getting the message that it could damage your brain, never really understood why. So let’s learn a little more.
What is a concussion?
Concussions are a type of traumatic brain injury that is caused by a hit to the body or head. In this collision the brain is jarred or shaken inside of the skull. This can cause confusion, dizziness, headaches, disorientation, and vision problems.[1] Depending on the severity of the concussion symptoms may seem to disappear within hours, days, weeks or months. However, even if the symptoms seem to have disappeared there still may be lingering effects in the brain.
So, “what happens to the brain when a concussion occurs?” you may be asking yourself. Concussions cause a great amount of stress on the neurons in the brain because there is an influx of calcium ions due to increased signaling as well as calcium accumulation. This accumulation can decrease the energy production in the brain by disrupting the mitochondrial process. On top of which, the concussion also causes a change in the regulation of potassium ions inside and outside the cell. Normally the concentration of potassium outside the cell is high and inside the cell is low, but when a concussion occurs the gradient changes and the potassium pumps must work extra to return it to regular levels using extra energy and creating an energy deficiency. This means that there may not be enough energy to support normal brain cell activity. The highest risk for lasting impact on the brain for concussions is while the first concussion has not fully healed. If the brain which is already working overtime to compensate for the repair from one concussion has the ion levels thrown off again, it may not have the energy to compensate for the second injury and can cause irreversible damage to the brain.
Kids and Contact Sports
Concussions have been a fairly hot topic over the last few years, especially when it comes to safety rules for athletes, young and old. Children take longer to heal from concussions and while they often wear more protective gear and don’t hit as hard as older athletes, safety is always a concern for parents, and rightly so.
A sport near and dear to my heart is hockey. We all enjoy a big check. It’s part of what makes the game unique and exciting, but it also brings one of the biggest health risks of the game, especially in terms of concussions.

There has been talk of not allowing checking in any level before high school hockey. For safety reasons, knowing that younger brains do not cope as well with concussive injuries, this in a way makes sense. On the other hand, if there is no checking before high school, freshmen are going to be thrown into a situation that they are not prepared for. In my opinion, wouldn’t it make more sense to teach checking, safe checking, at a young age before they hit as hard? Could this prevent some of the checking mishaps? Or do we just not allow freshmen to play varsity hockey for a while until they learn the checking game? Because a kid who may have the agility, stick- and foot-work ability of a varsity level will not be adequately prepared without the experience with the checking game.
It also begs the question whether or not kids should participate in contact sports at all. But sports provide exercise, energy release, and social opportunities that are important for physical and social growth.
Alcoholism: an Issue of Mind Over Matter?
To most of us, the notion that alcohol abuse is a huge problem in American society is not a new one; but if you’re anything like me, you didn’t fully understand or really care about the scope if the issue when going through the motions of the D.A.R.E. program in elementary school or later in required health classes, and you haven’t really thought about it since. Revisiting the topic, I was taken aback. The deaths, costs, and health problems attributed to alcohol abuse and alcoholism in the United States are enormous, effecting approximately 14 million people and costing $184 billion a year, according to the Tenth Special Report to the U.S. Congress on Alcohol and Health in 2000. For the U.S. population of that time, that was about 1 in 20 people effected… and that’s still a boatload of money. Advancement in the understanding of the pathophysiology and neurochemical pathways of alcohol abuse disorders has taken strides in recent years, but the questions of treatment method and viability still loom largely unanswered. What is the most effective target for pharmacological treatment? Should neurochemical means even be used in the treatment of alcoholism?

In alcoholism, alcohol preference and reinforcement seems to occur as a result of ethanol’s interaction with the dopaminergic (DA) signaling system. Ethanol decreases GABAergic activity; GABA is an inhibitory neurotransmitter, so a decrease in it makes signal transduction easier in the neuron – in this case, DA neurons. Thus, ethanol leads to an increase of dopamine release, and dopamine receptors are activated more, increasing adenylyl cyclase activity, which increases cAMP production, resulting in increased protein kinase A (PKA) signaling, which affects many substrates downstream, including DARPP-32 and CREB. DARPP-32 activation via PKA leads to NMDA receptor phosphorylation and activation, allowing an influx of Ca2+ into the cell which activates protein kinase C (PKC), finally resulting in an increase of the reward response associated with alcohol use. The effects of CREB, on the other hand, are associated with alcohol tolerance; an increase in CREB activation results in an increase in transcription of genes containing cAMP response elements, which decreases the reward response, making it necessary to consume more alcohol for the same effect. From these findings, it is suggested that DA receptor, DARPP-32, and PKC activation increase alcohol consumption, and PKA and CREB activation decrease alcohol consumption. Effective targets for pharmacological treatments may then be DARPP-32, PKC, and CREB, whose activities are abnormal in alcoholics, thought to be caused by genetic irregularities.
Researchers definitely have some leads on where to go with neurochemical treatments, but it is still unknown how effective these may be. It has been hypothesized that it is a combination of genetics and environmental factors such as stress that drive the development of alcoholism. Not only is this a possible cause for the disorder, but the researchers go as far as to suggest that the combination of these two factors is ultimately the only cause of alcoholism. If this is true, treating one of the factors should stop the progression of the disease and effectively nullify the dependence on alcohol. I’m not sure if it’s the most effective option, but I would favor treating the psychological factors such as stress and depression before resorting to chemical means. If you’ve read my past posts, you’ve probably discovered that I’m a minimalist when it comes to pharmaceuticals. So much of the time, chemical treatments only alleviate the symptoms of a disease and don’t get to the root of the problem, creating a dependence on the treatment instead of the treatment allowing a person to live free from the disease. In the case of alcoholism, it seems to me that only an alcoholic willing to receive help will effectively be treated, and at that point the most cost effective and personally empowering form of treatment involves helping them learn to cope with stress in healthy ways and work through whatever personal problems lead them to alcohol in the first place. Programs such as Alcoholics Anonymous have been effective for many people, and with the appropriate help and care, any alcoholic should be able to gain control of their life again. Kudos to the scientific community for their advancements in so many treatments for a wide variety of issues, but I think some things are better left to the power of a person’s mind.
Alcohol and the Brain
This week in class we discussed the affect of alcohol on the brain, specifically what does ethanol start when a cell is exposed to it. As it turns out there are many different processes which alcohol sets off in the cell. First we have adenylyl cyclase activating protein kinase A. This pathway is important because it leads to the activation of many different proteins within the cell and affects everything from the reward system in the brain to the breaking down of sugar. This happens when we see ethanol blocking type I equilibrative nucleoside transporters which leads to the accumulation of adenosine on the surface of the cell. This buildup leads to the activation of A2a receptors which increases the activity of adenylyl cyclase. This process is also important because it leads into why alcohol is so addictive. PKA eventually leads to the activation of a protein called CREB which expresses, that is activates the production of, several proteins that are involved in behavioral responses to various substances. The article also talks about a protein called DARPP-32 which allows dopamine receptors to remain active although ethanol by itself would otherwise inhibit the activation of such receptors.
Another important molecule that alcohol interacts with is called Fyn kinase. Fyn kinase’s function in the cell is to phosphorylate, which means in this case activate, the NR2B subunit of the NMDA receptor which thereby increases the receptor’s function. What happens when ethanol interacts with Fyn kinase is that the ethanol causes Fyn kinase to dissociate from a protein called RACK1, the job of which is to prevent Fyn kinase from doing its job. Once dissociated, the Fyn kinase is able to activate the NR2B subunit.
Another important molecule that the researchers in our paper believed that alcohol interacts with is protein kinase C which is involved in the building up of a tolerance to alcohol and the desire for alcohol. The researchers believe that PKC is preventing the suppression of GABA-A receptors by other proteins. PKC also affects glycine receptors, but the researchers are not yet sure about the mechanism by which this is done.
The last protein which the paper focused on is that of phopholipase D. Under normal circumstance, Phospholipase D turns the phospholipids that make up the membranes of your cells into phosphatidic acid which goes on to activate other processes in the cell, the activation of protein kinase C for example. What happens when ethanol is present is that the phospholipase D has a preference for ethanol over its normal target. Phospholipase D interacts with ethanol and creates phosphatidylethanol which isn’t as good of a messenger as phosphatidic acid was. Phophatidylethanol is also thought to be a cause of the tolerance which develops for ethanol’s intoxicating effects.
In our discussion group this week I found that our groups seemed to be most interested in the question of whether alcoholism is a biological problem or an environmental problem, that is to say whether it is an individuals fault for their alcoholism, or the fact of where they grew up. Our group seemed to agree that the environment in which the person lives plays the greatest role in the development of alcohol as we actually had two group members who were able to live in a country where alcohol consumption is much higher per capita than it is in the US. They said that drinking is done much more socially, rather than to feel the effects of the alcohol as quickly as possible. They also said that alcohol is a lot less taboo and that it is more expensive in those countries. They contrasted this with our own community where we drink to get drunk and there are enough drink specials going on with enough frequency that you could get drunk every night of the week if you wanted. Anyway, I agree with the rest of the group in that we could do a lot towards decreasing alcoholism if we changed the drinking culture.
I'm Cutting You Off! Treating Alcoholism
Alcohol consumption on a global level varies greatly from country to country, as well as the levels of alcoholism. The curious aspect is why some countries in Europe can consume more alcohol per capita yet the rate of alcoholism can be so much lower than it is in the United States. Alcoholism is a growing problem in the United States and methods of drug treatment are, interestingly, targeting the trigger receptors of craving that lead to relapse instead of what parts of the brain that are affected directly after alcohol consumption. Whether social change or new drug development, a plan for treatment option or fixation will happen.
![]()
Alcoholism is classically defined as having signs of physical addiction to alcohol and continuing to drink, despite problems with physical health, mental health, and social, family, or job responsibilities. Alcohol may control your life and relationships. From this standpoint, around 15.1 million Americans are considered alcoholics, which seems like a crazy high number, at least to me. This is a problem with overconsumption, to the point of being socially unacceptable. The social aspect of drinking is often how alcohol is consumed in Europe, which could explain the discrepancies between consumption and abuse between countries. Europeans maintain the mindset to consume a few drinks with their friends and family communally to elevate the level of enjoyment of socialization. Americans rely more on social drinking to alleviate stress and “escape” the week’s worth of stress on their Friday and Saturday nights. From this, it’s easier to see how problems could be developed from associating drinking with two different purposes. Americans associate alcohol as a problem-solver such that there is a greater chance real abuse and problems, like alcoholism could develop. The discrepancy in drinking ages between countries could also be a contributing factor.
Aside from the associated social aspects that could be contributing, researchers have been identifying a number of pleasure receptors that could be blocked to stop the chances of relapse and urges to consume. Such receptors include cannabinoids and opioids. Current drugs for alcoholism treatment target these receptors with the goal of preventing relapse and craving symptoms. This is interesting since they don’t prevent the effects of alcohol, which could lead to elevated levels of drinking, instead of curing. Instead, the drug treatments want to stop an alcoholic from consuming even just one more drink and alleviating the chances that they will by making cravings less frequent and less intense. The unfortunate side of this treatment method is that only small specific areas of the brain are responsible for these cravings, while these drugs target a whole host of areas in a kind of flooding technique. Additionally, these drugs have not been proven in trials to be entirely effective versus a placebo. Only about 20-30% of alcoholics are actually treated from drug treatments effectively. This is a shockingly small amount for a success rate. The hopeful method of increasing this is to begin to individualize methods of treatment to help each individual’s reasoning and craving triggers with more than just a drug treatment method. This is the hopeful future of alcoholism treatment, and hopefully, it will work for those who are beginning to suffer.
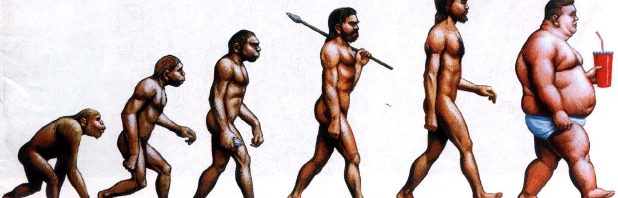
Obesity, Solved?
 Obesity has become a serious problem for the entire human race. Although it is more severe in developed countries such as the United State, both developing and underdeveloped countries are also suffering from obesity socially and economically. In the America, obesity has grown dramatically in the past fifty years. According to data reported by the CDC, the percentage of obese population has increased from 13% in 1962 to 35.7% in the year of 2010. Obesity can lead to many negative health effects such as cardiovascular diseases, and even neurodegenerative diseases (Alzheimer’s), which can result in gigantic medical expenses for our society. And since there are multiple dimensions to obesity, it is very important to investigate the causes of obesity from different perspectives.
Obesity has become a serious problem for the entire human race. Although it is more severe in developed countries such as the United State, both developing and underdeveloped countries are also suffering from obesity socially and economically. In the America, obesity has grown dramatically in the past fifty years. According to data reported by the CDC, the percentage of obese population has increased from 13% in 1962 to 35.7% in the year of 2010. Obesity can lead to many negative health effects such as cardiovascular diseases, and even neurodegenerative diseases (Alzheimer’s), which can result in gigantic medical expenses for our society. And since there are multiple dimensions to obesity, it is very important to investigate the causes of obesity from different perspectives.
In this week’s paper, we learned about the neurochemical mechanisms that are responsible for our appetite, which directly affect our food intake and therefore could be one of the biological causes of obesity. According to the paper, there are two types of neurons located in the arcuate nucleus of the hypothalamus that are affected by different levels of leptin and insulin in our body. When the levels of leptin and insulin in our body are high, the proopiomelanocortin (POMC) neurons are activated, and a-MSH is secreted. This will signal our body to reduce food intake and increase energy expenditure. On the other hand, when the levels of leptin and insulin in our body are low, the AgRP/NPY neurons will be activated and stimulate food intake. These results have been tested by the researchers, and the scientists from all over the world are trying to apply these informations to treatments of obesity.
Some might argue that weight problems are personal, and irrelevant to the society. And I respectfully disagree, in my opinion, obesity is a common problem for the society as a whole since it escalated to not just the personal health problem, but multi-dimensional. According to the former economist of the Qantas Airways, Tony Webber, the average weight for their costumer has gone up by 2 kilograms since the year of 2000. This means a 472 U.S. dollar increase in fuel cost for an A380 flying from Sydney to London, and nearly 1 million dollar increase in fuel cost for this particular line in a year. No wonder the airfares in general have skyrocketed so much. Furthermore, according to the Society of Actuaries, obesity has increased the medical cost in the U.S and Canada by nearly 130 billion dollars. All these facts suggest that obesity is a serious issue that needs to be dealt with as a society as soon as possible.
Is obesity the new norm for America?
Obesity and the many negative health effects that come with it have been growing rapidly in our society throughout the past decade. Our lifestyles have led us toward eating fast food for nearly every meal and go away from the now know as “old fashioned” home-cooked meal. Our society as a whole has also become so wrapped up in trying to do everything by sitting in one place, with our phones, rather than getting up and doing the physical activity to accomplish the task. Technology has been a very major factor in this rise in obesity as increases in technology have made it possible to get so much work done while simply sitting in an office as well as allowing kids to be entertained with video games for hours while sitting in one place. Each of these things I have mentioned and many more have led to the sedentary lifestyles that have become much more common in our society and ultimately leading to a more obese America. Now the real question is, what is causing this obesity, and is there any way we could come up with a way to prevent people from becoming obese?
In class we analyzed a scientific paper that looked at two of the main appetite hormones in the body and learned just what it is that they do to make us feel hungry or full. The paper itself went much more in-depth into the full mechanism of action for insulin and leptin signaling but I will briefly describe their effects. First of all, leptin and insulin act on two different neurons in the arcuate nucleus in the brain, the POMC neuron and the NPY/AGRP neuron. Decreased levels of insulin and leptin, ultimately stimulating food intake, stimulate the NPY/AGRP neurons. On the other hand, increased levels of insulin and leptin stimulate the POMC neurons, telling your body that it is full.
Now that we know a little bit about how our body works in terms of appetite we will be able to understand how fast food restaurants and other food companies can target our brain to make us eat even when our stomachs are full. With the increasing use of high fructose corn syrup (HFCS) in our society today some negative effects have also been exposed. HFCS is very cheap for food producers to use in their foods to make them taste much better. Since HFCS is so cheap it is used in nearly everything we consume today. This wouldn’t be such a big deal if it didn’t have such drastic effects on our appetite. HFCS actually decreases our levels of leptin as we eat making our bodies feel hungry even when we are full, ultimately causing us to eat much more than we should. This is a very bad thing as fast food chains can also use this to their advantage and sell more of their food that negatively affects our bodies.
Now the real question is what should be done about this growing problem in our society? It is very clear that there is a problem and scientists are researching different drugs that might be able to counteract this obesity and give people an easy way to stay thin while still eating all of these bad foods and living a sedentary lifestyle. I personally believe this would have very negative effects on our society. This would give people an easy way to avoid eating healthy and exercising, both things that are still very important when trying to live a healthy lifestyle. I think that a better option would be to promote healthy eating and exercising to kids as well as the parents of these kids in order to promote them to focus on maintaining a healthy lifestyle. It will be very interesting to see if scientists will in fact be able to come up with a pill that could stop obesity and just what sort of affect this would have on our society.
Obesity: A Growing Problem
When someone asks you to think of the stereotypical American, what is the first thing that pops into your head? If you’re anything like me, there will be a picture of an obese person walking down the street with a sugary soda in their hands. Obesity is a growing problem in America, and there are currently motions going across the nation trying to help reduce its severity. We all know that eating fatty and sugary foods is bad for you, but what chemically underlies the problem of obesity. This is the question we tackled this week in class.
Chemically, the problem of obesity lies within the chemicals leptin and insulin. Leptin comes from fat stores (adipose tissue) and insulin comes from the pancreas. These molecules are known for their signaling to the brain that conveys information about the fat stores within the body. These are released into the blood stream in proportion to the amount of fat and upon release, it will signal to reduce food intake. The problem of obesity comes in when they develop a resistance to these or there is an inherently reduced amount of signaling to begin with.
Since we know that there is a problem with the chemicals in the brain this leads us to wonder if there can be a drug that can help cure the obesity problem in America. To put it simply, there probably is. Nothing that has been used so far has been effective over long periods of time, but with more research done, there will probably be some “end all” pill on the market. Personally, I do not believe that this is the right step to take with this problem. Originally the problem still originates with us overeating unhealthy foods which will signal for more leptin leading to the resistance problem underlying obesity. In my honest opinion, I believe we need to redo how we eat. Stop buying the fast food and sugary snacks and start getting fruits and vegetables as well as becoming more active and getting off the couch. This may be a more expensive option, but in the end I believe that this will help stop the problem in a safer, healthier matter than using a magic pill. This solution may also help stop the corruption of the food industry and cause the government to stop subsidizing high fructose corn syrup and have them start subsidizing something a little healthier. This may be wishful thinking, but to me, this would be the best option.
Obesity Treatment: New Info, Old Answers
Musing about various life issues, I am often surprised at how little in my regular day I recognize concepts that are fairly obvious – things that I just haven’t taken the time to consider. One topic that falls into this category is that food is a ridiculously large part of our culture. Holidays revolve around meals, people bond when eating together, and people eat for fun and comfort, not just for sustenance. Food has become a pastime and entertainment, and it often signifies the importance of an occasion and sets a mood – it can be viewed as an art. In fact, I can’t really think of anything that’s as routinely and prominently celebrated as food, especially in American society. It may be due to this that we as a society have so many health problems relating to eating and nutrition; obesity and diabetes are two major issues that have been increasing in prevalence over the years and have gained attention as the foremost health problems in the US, as well as possible contributors to other diseases and disorders. Clearly, these are issues that need to be dealt with, but the question is, how?

Likely the most effective targets for treatment of obesity, especially, are the insulin and leptin signaling pathways, leading to a decrease in food intake to aid in losing weight. Insulin and leptin are hormones that play influential roles in energy intake and homeostasis; leptin in particular acts in the brain to signal the feeling of being full. The general pathway of insulin and leptin signaling in a well-functioning system starts with the digestion of food inducing the secretion of insulin from the pancreas and release of leptin from fat tissue. These hormones then travel through the bloodstream and activate receptors in a part of the brain that controls energy homeostasis via signaling related to food intake and metabolism. Neurons expressing the polypeptide proopiomelanocortin (POMC), when activated, will secrete the neuropeptide α-MSH which works to signal for decreased food intake and increased energy expenditure. Conversely, neurons expressing neuropeptide Y (NPY) and agouti related protein (AgRP) are activated by a decrease in insulin and leptin, resulting in signaling for increased food intake and decreased energy spending. Although similar in resulting cellular responses, NPY and AgRP work in different ways; NPY directly activates pathways which lead to increased food intake, whereas AgRP blocks the α-MSH receptor, inhibiting the pathway leading to decreased food intake.
The insulin and leptin signaling pathways themselves are also quite similar in cellular response, as they share a common downstream effector molecule – although the two receptors may have different primary effectors that begin two signaling cascades, these cascades converge on a single molecule and therefore share the ends of their pathways. The receptors’ primary effectors may have multiple signaling routes which do not converge with that of the other’s, but it has been shown that there exists at least one molecule on which signaling pathways from these two receptors converge. This indicates that there is a high level of cross-talk between the pathways of insulin and leptin, so a change in one highly affects the other.

Here’s the issue with the idea of manipulating the insulin and leptin systems to treat obesity and other diseases relating to overnutrition: long term treatment will only end in patients being dependent on it to maintain their weight, since a treatment directly affecting energy homeostasis will swing the energy balance the opposite way if discontinued. Diet pills notoriously give great results for weight loss in the short term, but after patients have stopped taking them, the weight comes right back and then some. I don’t believe that any outside treatment acting on the body for weight loss would be truly effective without lifestyle change – that is the necessary and lasting component to fitness and physical health. I support these pharmaceutical treatments for those who need help to achieve an initial weight loss in order to make exercise more feasible, but anything less than a necessity like that would only make things harder in the long term. Sometimes, if not often, the simple answer is the best answer – maybe appropriate nutrition and exercise are the cure-all for the health problems in today’s society.