According to the Center for Disease Control and Prevention website, “…. There has been an increase in obesity in the United States and rates remain high. More than one-third of U.S. adults (35.7%) and approximately 17% (or 12.5 million) of children and adolescents aged 2-19 years are obese”. Furthermore, apart from the health consequences of obesity, which includes, but is not limited to, coronary heart disease (CHD), type 2 diabetes (T2DM), and various cancers, obesity has direct and indirect effects on the nation’s economy. Direct medical costs incorporate the diagnostic and treatment services that are related to obesity, while indirect costs comprise of morbidity costs and mortality costs. To expand further, morbidity costs are defined as “the value of income lost from decreased productivity, restricted activity, absenteeism, and bed days.” Finally, mortality costs are the costs tagged on the future losses of income as a result of premature death.
These facts are unsettling. Clearly, intervention is needed, but at what point is government able to intervene? Does government intervention obstruct a person’s free will? Can the government dictate what items are sold in grocery stores, or how much a person can buy, or what ingredients can be used in products. The list of questions goes on and unfortunately, they are not easy questions to answer. However, what might help in answering these questions is the increasing amount of scientific evidence pointing to dysregulations in brain chemicals that contribute to obesity and obesity-related diseases. Due to the ongoing and increasing epidemic of obesity and diabetes in the US (and worldwide), scientists feel a sense of urgency to study insulin and leptin resistance. Growing evidence suggests that neuronal signals generated by insulin may overlap with signals activated by leptin, which would explain similarities seen in their effects.
Briefly speaking, both insulin and leptin work on neurons in the hypothalamus (as well as other locations in the brain). More specifically, insulin and leptin act on receptors found on neurons in the arcuate nucleus of the hypothalamus. One type of neuron found in this location is called a POMC neuron. They are activated by insulin and leptin to secrete a-MSH. When stimulated, the POMC neuron reduces food intake and increases energy expenditure. The other main type of neuron found in the arcuate nucleus is called an AgRP/NPY neuron. As opposed to POMC neurons, AgRP/NPY neurons are stimulated by decreases in insulin and leptin levels and stimulate food intake. AgRP/NPY neurons would be activated during periods of weight loss and prolonged absence of food in order to increase a person’s intake of food. After significant research, scientists have concluded that both insulin and leptin function as fat signals and have multiple similar physiological effects. Furthermore, insulin and leptin share their key sites of action in the hypothalamus suggesting that they have similar intracellular properties by which disruption in these pathways lead to resistance of their actions. Understanding the mechanisms by which these hormones affect energy homeostasis shows promise in promoting insight into practical and effective targets for therapy of obesity.
I think such therapies show more promise in treating the rising epidemic of obesity in the country. I am afraid that preventative courses of action obstruct a person’s free will more than therapeutic treatments in response to developed obesity do. Ideally, people would take responsibility for their own health in eating the right things and exercising daily, but evidence shows that this does not always happen. It remains clear that people need a more serious and invasive way to treat obesity. Without putting limits on what a person can or cannot buy, we need a way to counteract the negative effects that obesity has on a person’s lifestyle and the negative effects obesity has on society. I am hopeful that scientists are on the right track and will soon be successful in finding ways to counteract these effects. However, I also feel that such therapies will only be successful if paired with healthy dieting and exercise. Success does not come in simply administering a drug that works to decrease the nation’s high rates of obesity. Success comes when we reduce the nation’s obesity and promote education to prevent the further rise of obesity in the nation and stimulate the nation’s productivity.
Obesity: Who's to Blame? Who's Responsible?
Obesity is a problem that is worthy of more in-depth examination. The Centers for Disease Control and Prevention (CDC) states that more than a third of adults in the United States are obese (http://www.cdc.gov/obesity/index.html for more information on obesity). To me, the fact that weight should be discussed by an organization dedicated to the control and prevention of diseases is itself indicative of a problem. Weight is much more than a number, and it is much more than a description of someone. With connections between obesity and other diseases such as type II diabetes, stroke, heart disease, and certain types of cancer being made, we need to take our weight very seriously. And this isn’t just a personal problem. The additional cost of being obese is another thing that should make one take notice of the problem.
What are the causes? There are a variety of causes that span social, economic, racial, gendered, personal, and societal sources. Many are quick to implicate the prevalence of fast food when the obesity epidemic is mentioned. As modern lives become even more fast-paced, families have such variant schedules as to make family meals a norm of the past or special weekend occasion, and instant gratification is reinforced on many levels, fast food has definitely becoming an appealing option to many. The changes in food processing may also be to blame. Preservatives, artificial flavoring and coloring, high levels of sodium and fat, and the use of high fructose corn syrup have all come under attack in recent years. These elements not found naturally in food are being processed differently by our bodies and the products are being metabolized differently. The effects on our organs, including our brains, should be noted. Signals to the brain are not being transmitted correctly, nor are the signals that are there being received properly. These signaling errors can have disastrous effects.

How can this problem ever be resolved? Just as there are several causes of obesity, so too can there be several solutions to this problem. Better diet and exercise seems to be an overly simplistic solution, but it is crucial and widely recommended. Other solutions including many diet programs, weight-loss drugs, and hormone therapies encourage and are often more effective when combined with a balanced diet and exercise. A 2003 article examines the legal implications that may exist between obesity and the fast food industry (http://content.healthaffairs.org/content/22/6/207.full), bringing up ethical issues of negligence and failure to warn. Two recent proposals by the FDA would establish requirements when it comes to labeling, ingredients, and caloric intake (http://www.fda.gov/Food/LabelingNutrition/ucm248732.htm). Some insurance companies have established a policy of providing discounts or rebates to individuals that have a gym membership. Could a similar precedent be made for individuals that shop for organic, local foods or participate in a farmers’ market?

Where does this information leave us? Clearly, there is enough blame and responsibility to be shared by many if not all. While it is easy and makes sense to say it is the responsibility of the individual to make sound choices when it comes to health and wellness, it isn’t that simple. The cheapest food option tends to be the quickest and most available option for consumption. When social, economic, racial, and other prejudices and predispositions are considered, it is difficult to conclude that an individual is completely in control of decisions related to health and wellness. Many options exist, but they are not all available to each person. Obesity can be examined under the lens of several different social constructs, and only when we are ready to address each obstacle will we be able to improve the quality of life for many.
The Epidemic of America…Obesity
Obesity is a major problem in the USA but how much of it’s onset is due to actual physical problems and how much is due to the fast paced world we live in and perhaps laziness? This week we talked about leptin and insulin’s signalling in obesity. The first question asked by our discussion leaders was in the fast paced world we live in, is it more important to develop an anti-obesity drug or to promote healthy eating habits and exercise? Personally I believe that the major cause for obesity is the convenience of being lazy and being able to live in such a way. I think promoting a healthy lifestyle is the best course of action because not only will the rate of obesity be declined but all the benefits of a healthy lifestyle will enter into the lives of Americans, quality of life in America will increase and I feel that exercise and healthy diet are the best way to achieve that.
Another big topic we touched on was the use of high fructose corn syrup (HFCS) in countless foods we eat nowadays. Leptin and insulin are signals in the body that tell us when we are full and when we are hungry. HFCS slows the release of leptin causing us to not to know when to stop eating and thus makes us eat more than we need. The question was whether the government should regulate the use of HFCS or should the food companies be morally obligated to preserve human health. I think that again the answer lies with the consumer and not the government or the food companies. The reason HFCS is used in so many things is because the government rewards farmers for growing it, thus making it cheap to use. If the government regulated the use of it they would have to stop subsidizing it and thus make it more expensive to use, thus making everything more expensive and making a lot of food unattainable to families that are poorer. Again the answer is to promote better living habits because that will keep HFCS cheap while still reducing obesity.
The last big topic we covered was whether leptin resistance or the addiction to food had the major effect on obesity. What this meant was whether we thought that something was physically wrong in people with obesity or whether obesity was effected more by the fact that people get addicted to the taste of the food that they can’t stop eating it. I think that it is a combination of both. To be more exact I think that one causes the other which in turn causes the first to occur more. What I mean is that people get addicted to the taste of food or eating itself, which causes the increased consumption of HFCS which causes leptin to be released slower, which causes you to eat more which increases consumption of HFCS…etc. The only way I can think of fixing this aspect of obesity would be making food taste bad but let’s be honest that just isn’t going to happen.
The Brain and Obesity
This week in class we talked about how the brain functions in your body’s search for food, specifically how the brain controls your appetite and how if there is a defect in the system, the body can rapidly put on a lot of weight. What basically happens in your body is this, insulin and leptin are secreted in proportion to the amount of fat cells in your body. These two molecules, called adiposity signals, will in normal cases be secreted in larger amounts and cause you to feel less hungry when your fat stores are sufficient, that is that you have adequate access to food, and be secreted in smaller amounts making you feel more hungry when your fat stores are deficient, when you aren’t taking in enough food. These two molecules do this by acting upon the hypothalamus within your brain, specifically on the region of the hypothalamus called the hypothalamic arcuate nucleus. This nucleus contains two kinds of receptors for leptin and insulin that have opposite effects on the body. The proopiomelanocortin(POMC) receptor when activated by insulin and leptin secrete a molecule called alpha-MSH that causes your body to reduce its food intake and increase the amount of energy that it uses. The neuropeptide Y(NPY) and agouti related protein(AgRP) receptor on the other hand cause your body to increase its food intake and make its uses of energy more efficient.
Here’s where the article turns to obesity. If there is any sort of malfunction within this system, we see continued food intake even with ample fat stores. The article says that there are mutations where certain parts of the system were never created by your body, the more common reason why the system ceases to function is that neurons within the hypothalamic arcuate nucleus develop a resistance to leptin and insulin. This happens because that the receptors activated by leptin and insulin lose their ability to activate a molecule called PI3K. In insulin signaling PI3K is activated by insulin-receptor-substrate(IRS) proteins. These proteins are activated when they recieve a phosphate molecule from the insulin receptor itself. It can be assumed that something similar is happening in leptin signaling.
For our discussion this week we talked exclusively about the relationship between this system and America’s obesity epidemic. We agreed that it would probably be best that we didn’t focus on a silver bullet solution to this problem, aka some sort of anti-obesity medication. We said that instead we should really focus on instilling an active lifestyle in people as if you removed the one outward sign of overeating, you would not encourage people to eat anymore healthily. On a similar note we also agreed that the food industry is somewhat to blame in the obesity epidemic as it is not their responsibility to make people make healthier choices, but to make people buy more of their product. The use of high fructose corn syrup for one is a huge problem as it is very cheap and has been found to negatively interact with your appetite. For sure, this is definitely going to be a problem with no easy answer and it is probably going to have to come down to people taking responsibilities for their actions. I mean, this is probably the first time that average life expectancy for a generation is going to be less than the generation before it, I don’t think that that is a legacy that a generation wants to leave behind.
Bipolar Disorder Treatment: a Work in Progress
Bipolar disorder (BD) is a neurological disease that intrigues me to no end. There have been multiple mechanisms proposed and some groups seem to be on promising tracks to a definitive answer, but as far as I can tell, people are still just grabbing at straws. The treatment thusfar for this disorder has largely been developed in a guess-and-check manner, which really makes me give an eyebrow raise. Drugs are developed, tested, and if they give the desired result in regards to symptoms expressed, they can be approved for treatment without having a good grasp on what chemistry is actually going on in the brain. Nothing like popping a fistful of Tylenol to get rid of that particularly nasty headache, not realizing its harmful effects on the stomach. We should strive for the ideal of fully understanding the processes involved with using a drug before implementing them – otherwise, we may be slowly killing ourselves.

The best explanation scientists have come up with involves arachidonic acid (AA) and its effects and regulation in the brain. Although multiple alleles have been linked to the development of BD, the heart of the action of the disease is hypothesized to stem from an overexpression or overactivation of AA, leading to neuronal damage via inflammation and excitotoxicity which eventually results in apoptosis and cerebral atrophy. This overexpression could be due to a number of dysregulations, including increased activation of neurotransmitter receptors that use AA as a second messenger, or a decrease in regulatory compounds such as docosahexaenoic acid (DHA) – an omega 3 fatty acid. Researchers have come to the conclusion of AA involvement by examining the similarities and differences between different BD drug treatments’ mechanisms, although these drugs’ mechanisms are not fully understood either.
Although the ideal is the goal, as in all situations reaching the ideal is admittedly difficult, if not impossible to attain. In the time it takes to carry out research to fully understand a disease, treatments are necessary to help those who need help now and can’t wait for scientists to make a breakthrough. My issue with the treatments researchers have come up with is that they almost all focus on medication, many of which have nasty side-effects. If scientists have an idea of what may be happening in BD, why not look just as hard into homeopathic treatments, which could potentially be more synergistic with our bodies and with less side-effects? Diet has a tremendous effect on the well-being of our bodies, including the development of neurological diseases. In the case of BD, an abundance of AA and perhaps a lack of DHA seem to be to blame, both of which are attained through one’s diet, either directly or through the acids’ precursors. Sure, it may take more work on the patient’s part, but this seems like a method to get closer to the crux of the problem, rather than giving patients almost literally a cocktail of medications with a boatload of side-effects. Call me crazy, but I believe the diet to be a very powerful thing.

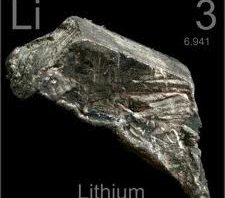
Is Lithium really the best treatment for bipolar disorder?
Bipolar disorder is a major medical disorder that affects almost 14 million people in our U.S. today. This disorder might not be seen as a major medical issue to the general public as many people have never been exposed to a person suffering from BD, but it drastically affects individuals’ lives both mentally and socially. Bipolar disorder is characterized by rapid changes in mood, consisting of cycles between mania and depression. After analyzing the scientific paper titled, “Bipolar disorder and mechanisms of action of mood stabilizers” in class throughout last week and discussing with classmates, many interesting issues were cultivated.
The paper explained BD and outlined different hypothesis that described how the common drugs, including, lithium, valproic acid, and carbamezapine work in treating BD. The two main issues that stuck out to me after reading this paper was the fact that the cause of BD is somewhat of a mystery to scientists as well as the drugs used for treatment. Even though scientists have a few different drugs or drug combinations to subscribe to patients suffering from BD, these drugs could be dangerous to patients with long-term use.
The first very interesting topic that was brought up in classroom discussion was dealing with the current treatments of BD and their long-term effects on patients. BD is a very serious disorder that can cost patients a significant amount of money through treatment with drugs in order for them to live a normal life. Although there are drugs out there that treat BD fairly well, there are some very negative side-effects that come with taking these drugs for extended periods of time, and unfortunately, life-long drug use is necessary for most BD patients to live normal lives. Lithium is drug of choice for doctors as of right now even thought it has some negative effects on patients. With long-term use of Li, a patient can gain a very significant amount of weight and is also susceptible to the development of diabetes. Both of these can decrease the life span of BD patients. Although treating patients with Li can decrease life span, can they function without treatment?
Another interesting issue that stuck out in my head while reading through this paper was the unknown cause of BD. Although scientists have developed drugs to treat BD, they haven’t been able to identify a definitive cause to the life-changing disorder. Before reading the paper I thought that the cause of BD was primarily a genetic disorder. However, there are many different things that come into play when looking at what causes an individual to develop BD. The paper stated a very interesting statistic showing that only 40% of monozygotic twins both develop BD and less than 10% of dizygotic twins both develop the disorder. This emphasizes the fact that there must be another reason for an individual to develop the disorder.
The paper also talked about a recent genome-wide associated study that revealed 88 different alleles that increase the risk of an individual to develop BD. They also stated that a person with a combination of 15 or more of these different alleles has a significantly higher risk of developing the disorder. This doesn’t mean that someone with 15 of these alleles will definitely develop BD but it makes it easier for environmental factors to trigger the onset of the disorder. It seems as if the environmental aspect of triggering this specific disorder plays a very significant role in development of BD. Repeated findings have shown that half of the adults studied with BD reported having a traumatic/abusive experience as a child. This highlights the fact that environmental factors can really play a part in developing BD.
Throughout classroom conversation someone brought up the interesting topic about testing children’s genomes to determine their risk of developing BD. Would knowing your child had a greater risk of developing BD change how parents raised their children? This was just an interesting question that is very controversial, as many other medical genetic topics are.
The topic of BD is a very mysterious topic that is being researched extensively by scientists in an attempt to both; determine the overall cause of the disorder, as well as developing a safer treatment for BD. It will be very interesting to see the progression of research and whether or not we can find a way to allow people living their lives struggling through manic and depressive mood swings to live a normal life without having to take combinations of drugs that could affect their future.
Bipolar Disorder: A Disorder with No Face
70% of Bipolar disorder patients are initially misdiagnosed. Bipolar disorder, also known as manic-depressive disorder, is  characterized by dramatic changes in mood. These mood shifts are significant because they drastically impair a person’s quality of life. The mood switches occur between a state of depression and various states of mania. Mania, an abnormally elevated or irritable mood, in bipolar disorder can occur in the form of mild mania, hypomania, or full-blown mania, with side-effects such as: hallucinations, catatonic behavior, aggressive behavior, and many more. This variance in mania led to classification of two different types of bipolar disorder. Type 1 bipolar disorder is diagnosed based upon one or more recorded incidents of mania with frequently occurring depression. Type 2 bipolar disorder is characteristic of hypomanic episodes, usually unknown to or denied by the person afflicted with the disorder, along with major periods of depression.
characterized by dramatic changes in mood. These mood shifts are significant because they drastically impair a person’s quality of life. The mood switches occur between a state of depression and various states of mania. Mania, an abnormally elevated or irritable mood, in bipolar disorder can occur in the form of mild mania, hypomania, or full-blown mania, with side-effects such as: hallucinations, catatonic behavior, aggressive behavior, and many more. This variance in mania led to classification of two different types of bipolar disorder. Type 1 bipolar disorder is diagnosed based upon one or more recorded incidents of mania with frequently occurring depression. Type 2 bipolar disorder is characteristic of hypomanic episodes, usually unknown to or denied by the person afflicted with the disorder, along with major periods of depression.
Bipolar disorder is becoming a more common disorder among young people with an average age of onset being 25. Although research into the treatment of bipolar disorder is promising for the betterment of extending the quality of life of young, because the disorder only afflicts 5% of the total U.S. population funding for bipolar research is small. Another factor which road blocks research into treatment options for bipolar disorder is the fact that the exact causation of bipolar disorder is unknown. Fact ors such as genetics, physiology, and environment all have an effect on the development and on-set of bipolar disorder.
ors such as genetics, physiology, and environment all have an effect on the development and on-set of bipolar disorder.
Treatment of bipolar disorder using FDA approved medication involves focusing on one aspect of bipolar disorder, that is mania. I was quite shocked when I read this fact. I found it surprising that an FDA licensed treatment of bipolar disorder is only required to treat one portion of the disorder and can ignore the other. In order to counter the manic episodes of bipolar disorder the most commonly used drugs are mood stabilizers, such as lamotrigine and carbamazepine. Mood stabilizers are used in treatment because they increase levels of GABA, a major inhibitory neurotransmitter, which reduces reception of dopamine, serotonin, and glutamate neurons. These neurons are excitatory and cause the perception of uplifting, “good” feelings. Mood stabilizers would thus inhibit the over-expression of “good” feelings, thereby taming the manic state in bipolar disorder. The most prescribed mood stabilizer is Lithium. Other treatments for bipolar disorder, which are less effective than mood stabilizers, are antipsychotics and antidepressants.
Further research should be conducted on bipolar disorder in order to not only cure the disorder but also off er researchers a better understanding of how the brain works. The problem facing bipolar disorder research is the fact that the number of people afflicted with the disorder is smaller than other disorders/diseases such as Parkinson’s Disease, Alzheimer’s Disease, depression, and schizophrenia. However, it should be noted that Parkinson’s Disease received little attention, in terms of funding for researching the cure, until Michael J. Fox became a spokes person for the awareness of Parkinson’s Disease. Therefore, if more attention is brought to the forefront of the U.S. people then surely funding for bipolar disorder would improve. There are notable celebrities who have bipolar disorder Russell Brand, Robert Downey Jr, Carrie Fisher, Kevin McDonald, Ernest Hemingway, Mel Gibson, Amy Winehouse, and Catherine Zeta-Jones. These celebrities could do wonders for bringing attention to the research of bipolar disorder if they became figureheads for living with the disorder just as Michael J. Fox did for Parkinson’s Disease.
er researchers a better understanding of how the brain works. The problem facing bipolar disorder research is the fact that the number of people afflicted with the disorder is smaller than other disorders/diseases such as Parkinson’s Disease, Alzheimer’s Disease, depression, and schizophrenia. However, it should be noted that Parkinson’s Disease received little attention, in terms of funding for researching the cure, until Michael J. Fox became a spokes person for the awareness of Parkinson’s Disease. Therefore, if more attention is brought to the forefront of the U.S. people then surely funding for bipolar disorder would improve. There are notable celebrities who have bipolar disorder Russell Brand, Robert Downey Jr, Carrie Fisher, Kevin McDonald, Ernest Hemingway, Mel Gibson, Amy Winehouse, and Catherine Zeta-Jones. These celebrities could do wonders for bringing attention to the research of bipolar disorder if they became figureheads for living with the disorder just as Michael J. Fox did for Parkinson’s Disease.
References:
http://www.statisticbrain.com/bipolar-disorder-statistics/
http://www.psychiatrictimes.com/bipolar-disorder/content/article/10168/53771?pageNumber=1
http://www.mental-health-today.com/bp/famous_people.htm
Images Courtesy of Google Images
Bright Side, Dark Side- Bipolar Disorder

Most people experience emotional ups and downs during the course of their lifetimes. Depending on either the events happening in our lives, or hormonal changes during different developmental stages, a typical person could experience quite a bit of mood fluctuations. But patients with bipolar disorder experience greater and more frequent mood swings than the typical person. Unfortunately, the mechanism of this disorder is not yet fully understood and therefore there are no physiological tests that could help diagnosing the disorder. And since it is sometimes very difficult to tell the differences between normal mood swings and symptoms of bipolar disorder, many people suffer for years before the illness is properly diagnosed and receive treatments.
There are three main hypotheses on the mechanism of the mood stabilizers that are widely recognized and greatly investigated by scientists, the “myo-inositol depletion hypothesis”, the “GSK-3 inhibition hypothesis” and the“arachidonic acid cascade hypothesis”. In the paper we read for this week, the authors focus on the AA cascade hypothesis and discuss the possible
mechanism for the action of mood stabilizers such as lithium, carbamazepine, sodium valproate and lamotrigine. Since some of these four drugs are channel blockers, and lithium is in its ionized form, they all have different properties which increase the difficulty to explain all four of them through one common hypothesis.
Arachidonic acid is a polyunsaturated fatty acid that is esterified predominantly in the stereospecifically number 2 position of brain membrane phospholipids. When released by a phospholipase A2 (PLA2), AA has multiple biological effects including neurotransmission, membrane excitability, long-term potentiation, gene transcription, membrane fluidity, neurite outgrowth, cerebral blood flow, sleep, memory and behavior. And according to the paper, the experiments show the four different drugs that are known to have positive effects on treating bipolar disorder all down regulate the AA cascade and even though they work at different levels of the cascade, their effects all contribute an overall reduction of the AA turnover rate. These are promising results which will encourage the scientists to look into the this AA cascade even further in order to get a better understanding of what actually goes in terms of bipolar disorder. And hopefully come up with better treatment which will get rid of some of the nasty side effects of these current medications.
It is very difficult to imagine how it must feel like to live with suc
h a disorder, or to live with someone suffering from it. Although I am not an expert in psychiatry, personally, I believe that nature is in favor of everything being balanced. For example, human body prefers to retain hemostasis, any fluctuations of our body temperature, hormone levels, and even neurotransmitters could potentially cause major defects. It should be the same for our mind as well. A healthy mind, in my opinion, should be in a fairly stable mental state which one can function at his/her best.
Is Bipolar Disorder important? Is it even a real disease?
 Many people are affected by Bipolar Disorder (BD), a real, major medical and social burden. We may tease our peers, friends, or family about the disorder claiming they MUST have some form of it as they change moods so quickly. This is actually believed to be brought on by some physiological problem that has yet to be agreed upon. Doctors and scientists characterize the disorder by repeated periods of mania and depression or hypomania and depression. Victims of BD are heavily burdened as they are subject to deep depression without any real cause and even the opposite; they can be extremely happy without cause. Fortunately, there are treatments that have been used for decades such as lithium salts that are able to stabilize a person’s depression and mania symptoms. The problem is that scientists do not have a complete understanding of what causes the disease or how treatments that are available actually work to subdue the mood swings of BD patients. Should we put more money and efforts into treating this disorder or focus on diseases that are life-threatening such as Alzheimer’s, Parkinson’s, and Huntington’s disease?
Many people are affected by Bipolar Disorder (BD), a real, major medical and social burden. We may tease our peers, friends, or family about the disorder claiming they MUST have some form of it as they change moods so quickly. This is actually believed to be brought on by some physiological problem that has yet to be agreed upon. Doctors and scientists characterize the disorder by repeated periods of mania and depression or hypomania and depression. Victims of BD are heavily burdened as they are subject to deep depression without any real cause and even the opposite; they can be extremely happy without cause. Fortunately, there are treatments that have been used for decades such as lithium salts that are able to stabilize a person’s depression and mania symptoms. The problem is that scientists do not have a complete understanding of what causes the disease or how treatments that are available actually work to subdue the mood swings of BD patients. Should we put more money and efforts into treating this disorder or focus on diseases that are life-threatening such as Alzheimer’s, Parkinson’s, and Huntington’s disease?
BD is a disorder that affects the life of its victim severely when left untreated. These people will experience mania symptoms such as feeling jumpy or wired, talking fast and incoherently, being easily distracted, sleeping little, being restless, etc. Those in the depressive state will experience feelings of worry and emptiness, feeling tired or slowed down, thoughts of suicide, etc. Adding to this the victims will switch between these two states sometimes often or they sometimes can remain in one state for a year or longer. This causes huge social problems. Those suffering from BD will have trouble maintaining relationships with friends and family and developing new ones. Their jobs will also most likely be affected, differently in the separate states of mania and depression. Despite all of these negative aspects of the disorder, in most cases it has been shown to be treatable. If patients stick to their polypharmaceutical regimen they are able to function normally and live average lives. If they are able to live normal lives with treatment then why are we still researching the pathology of the disorder? Why should we not focus on more pertinent diseases that are more life-threatening?
Diseases such as Alzheimer’s, Parkinson’s, and Huntington’s are thoroughly researched with their pathologies being partly understood and scientists are well on their way to a complete understanding of specific, central aspects. This is only half the battle. As research progresses and as scientists gain more knowledge, more is understood about how to either slow the degeneration of the disease or treat its symptoms. Even better, we are always progressing to a hopeful cure for each of these diseases. Each of these lead to eventual deaths because of their symptoms, malfunctions of neurological pathways, and accumulation of unwanted masses in the brain. Should we focus on treating a disease such as BD when there are much worse diseases still in need of complete understanding? Many make the argument that many of the patients of these deadly diseases are no longer able to greatly contribute to society anyways so we should put our time and money into disorders like BD to increase productivity of these younger members of society. Either way, the whole argument is heavy in ethics and morals.
In my opinion, because we already have a working treatment, we should throw Bipolar Disorder on the back burner while we focus on diseases that are taking lives. If more money and efforts are taken and added to the research for Alzheimer’s, Parkinson’s, Huntington’s and other diseases like them we can hopefully come to a conclusion more quickly. From this we can create better treatments; a cure wouldn’t be unwelcomed either.
Exploring Mood Stabilizers for their use in Bipolar Disorder
This past week in class we discussed the various medications being used to treat bipolar disorder. In the article we were assigned to read for the week, it discusses what exactly bipolar disorder is, how the disorder is treated, and the most plausible explanation for what is occurring in the brains of those affected by bipolar disorder.
There are two different types of bipolar disorder, bipolar I which is characterized by alternating periods of mania and depression, or bipolar II which is characterized by alternating periods of hypomania and depression. The disorder itself is linked to multiple different genes within the human genome. There are 88 different risk alleles, or genetic sequences, that are present in those with bipolar disorder. If someone has fifteen of these sequences then they are at a significantly higher risk than the general population. Besides the alternating cycles of moods, bipolar disorder brings with it many other health problems. Bipolar sufferers often take up smoking or substance abuse in their manic phases. The treatments for this disorder can bring on obesity and diabetes in the patient. Perhaps one of the worst things facing a bipolar disorder sufferer however is the increased chance of suicide that they face which is 10 to 20 times the rate among the general population.
As for the treatment of Bipolar Disorder, doctors use a technique called rational polypharmacy, which pretty much amounts to treating new symptoms as they pop up with various mood stabilizers, antipsychotics, antidepressants, and hypnotic benzodiazepines.
And this really only gets to the heart of the matter in that researchers do not really know yet what the root causes of Bipolar Disorder is, but they think that it has something to do with arachidonic acid. The theory here lies in that the chemicals that are used to treat the symptoms of bipolar disorder are interfering with the actions of arachidonic acid in the cell. Therefore, the researchers believe that the chemicals are correcting a chemical imbalance with regards to arachidonic acid.
For our discussions this week we talked about treatment of bipolar disorder and what it means for society. We talked about what it would mean for society if we found a cure for Bipolar Disorder, or more to the point if we even needed to find a cure immediately. We had the good luck to have two people who have happened to know someone with bipolar disorder and they both agreed that the disorder does not really affect them that much as long as they stay on their medications. This kind of segued into our next discussion question about the affects on the body that mood stabilizers have, namely obesity and diabetes and if these could possibly be worse side effects than the others because they could contribute to the depression that is felt by sufferers. I think we agreed in the end that this is merely a matter of adaption the same as learning to take all of your medication, the sufferer needed to take into account the weight gain that they would experience in the course of their treatment. I think the most interesting conversation we had however was about mood itself, namely are we misdiagnosing bipolar disorder in people who are just emotional. Like could we possibly be medicating people who are not like bipolar disorder sufferers in that their mood swings are chemically induced, but that the mood swings that these people experience are the result of them being more open with their feelings than the rest of us. It made me for one wonder whether as a society we use drugs to help people, or to make them more like the rest of us. I mean you have to take into account people who suffer from some sort of mental problems, but contribute so much to the arts and sciences.
That’s all for this week, next week’s topic will be the relationship between leptin and obesity