What is a psychopath?
Most likely when you think of a psychopath, you probably think of a person like Jeffrey Dahmer, Ted Bundy, and John Wayne Gacy. Although they may be categorized as psychopaths, what actually defines them as such? Yes, they were serial killers, but that’s not a required “symptom” of a psychopath. So, what is a psychopath then?
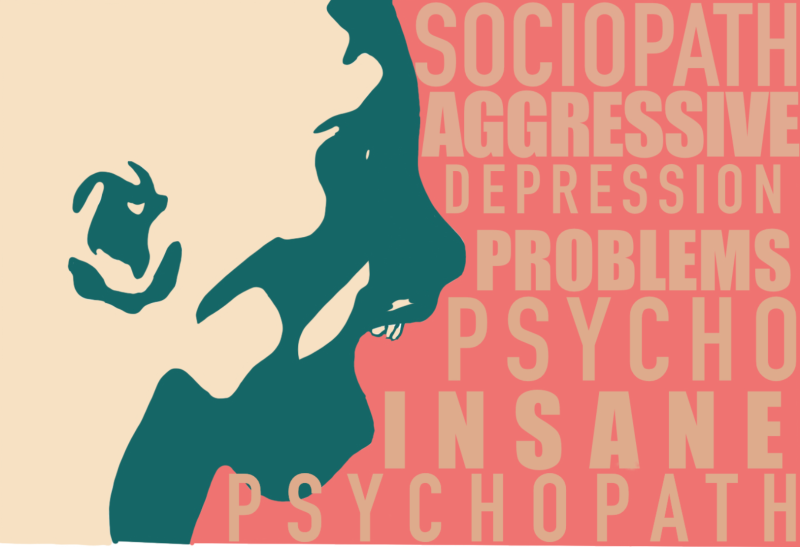
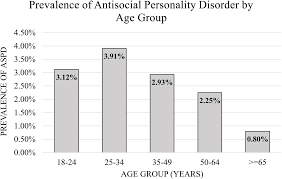
Psychopathy is a very extreme form of antisocial personality disorder (ASPD). A person cannot be given the diagnosis of psychopath, those are merely traits given to a person who suffers from ASPD. ASPD is just one of the ten types of personality disorders. The Diagnostic and Statistical Manual of Mental Disorders defines ASPD as an individual who shows a continued pattern of disregard and violation of other peoples rights, emerging around the age of 15 with three or more of the following symptoms:
- Repeatedly breaking the law
- Repeatedly lying for personal gain or pleasure
- Impulsivity
- Irritability and aggression towards others
- Reckless disregard for the safety of others
- Consistently irresponsible
- Lack of remorse
:max_bytes(150000):strip_icc()/what-is-a-psychopath-5025217-62ac72329fee4a16b4bad6f1980c421f.png)
When we talk about any personality trait or quality a person has, scientists like to refer to the “nature” of the person as well as the “nurture.” Nature refers to the biological makeup, or the genetics a person has. Nurture, on the other hand, is how a person grew up, how they were treated as a child, and their life experiences. Figure 2, below, shows these contributing factors. It’s believed that both nature and nurture contribute to the life of a psychopath. Although there is a strong biological component, which will be explained later on, there are also environmental factors that contribute to this disease. Some of these factors may be neglect, abuse, and poor parenting.
:max_bytes(150000):strip_icc()/2795392-article-what-is-nature-versus-nurture-5a971887eb97de0036685ad3.png)
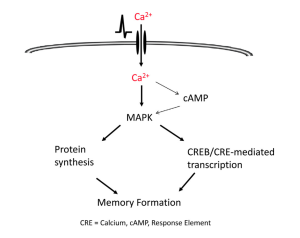
Neurobiological Roots of Psychopathy
When determining what could be going wrong in the brain, researchers found that those who were diagnosed as antisocial with psychopathic traits showed abnormal glucose metabolism and opiodergic neurotransmission in their brain. Abnormal glucose metabolism that leads to hypoglycemia has come to be one of the strongest predictors for violent crimes. One study followed individuals for eight years, hypothesizing that decreased glucose uptake in the prefrontal cortex of the brain led to violent crimes being committed by antisocial males. Over this eight year period, researchers were able to determine that 27% of the violent crimes could be explained by the decreased glucose uptake. From this study, researchers determined that substances that increase glycogen formation and decrease the risk of hypoglycemia could act as potential treatments for impulsive violent behavior.
Conclusion
Labeling someone as “psycho” or “crazy” is something many people do. But, neither of those terms are diagnoses. If a person truly is “crazy,” they most likely suffer from an antisocial personality disorder with psychotic features. Nature and nurture both play a major role in understanding what creates a psychopath. But, most importantly, there are multiple neurobiological roots that contribute to this disease. Glucose metabolism, and opiodergic neurotransmission are two that researchers know about currently. Knowing whether or not there is more that contributes to the root of psychopathy isn’t quite known but researchers hope to understand more in the future.
References:
Antisocial Personality Disorder: Often Overlooked and Untreated
Low Blood Sugar (Hypoglycemia)
Low non-oxidative glucose metabolism and violent offending: An 8-year perspective follow-up story
Neurobiological roots of psychopathy
The role of the opioid system in decision making and cognitive control: A review

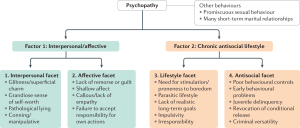 When diagnosing psychopathy, a questionnaire called the
When diagnosing psychopathy, a questionnaire called the 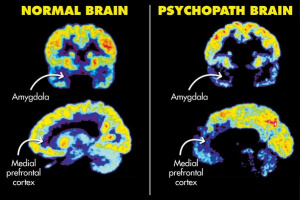 Researchers do not know much about the true cause of psychopathy and ASPD. Previous research has shown that there may be some
Researchers do not know much about the true cause of psychopathy and ASPD. Previous research has shown that there may be some  There are many stereotypes when it comes to the term psychopath. Most of these stereotypes come from media. Most notably, Joe Goldberg from the hit TV show You and Norman Bates from the hit TV show Bates Motel. The TV and movie industry has made a lot of money off of dramatizing people and the term psychopath, but these are not an accurate depiction of what it is like to live with the psychopath label (Norman and Norma Bates on the left and Joe Goldberg below).
There are many stereotypes when it comes to the term psychopath. Most of these stereotypes come from media. Most notably, Joe Goldberg from the hit TV show You and Norman Bates from the hit TV show Bates Motel. The TV and movie industry has made a lot of money off of dramatizing people and the term psychopath, but these are not an accurate depiction of what it is like to live with the psychopath label (Norman and Norma Bates on the left and Joe Goldberg below).
 Artstract #2
Artstract #2







:max_bytes(150000):strip_icc()/the-four-stages-of-sleep-2795920_FINAL-5c05c2fc46e0fb00018dac3d.png)

:max_bytes(150000):strip_icc()/how-to-get-better-sleep-5094084-regular-FINAL-2c371001cada4ad391f6de53fc6053c9.png)