As I sit down to write my final blog post, I’m struck by how much this class has not only deepened my understanding of brain chemistry but also reinforced the core values of Concordia. The CORE curriculum—built on the idea of Becoming Responsibly Engaged in the World (BREW)—has shaped my academic journey in ways I couldn’t have anticipated when I first stepped onto campus. This neurochemistry course, in particular, has been a powerful synthesis of scientific rigor, real-world applications, and collaborative learning, all of which align with Concordia’s five goals for liberal learning.
- Instilling a Love for Learning
One of the most profound lessons this course has taught me is that learning doesn’t stop at memorizing pathways or neurotransmitters—it’s about curiosity, questioning, and connecting ideas across disciplines. Neurochemistry is an inherently dynamic field, with new discoveries constantly reshaping our understanding of the brain. Whether we were discussing neurodegenerative diseases, synaptic plasticity, or the biochemical basis of psychiatric disorders, I found myself constantly wanting to dig deeper. Each week as I wrote my Wiki page, blog post, and prepped for the small-group discussion, I found myself immersed in the topic of the week, often falling down rabbit holes and reading far beyond the article for the week. I truly enjoyed learning more and more about each topic. That intellectual engagement is what liberal learning is all about: not just absorbing information but actively pursuing knowledge with enthusiasm.
- Developing Foundational Skills and Transferable Intellectual Capacities
This course sharpened skills that extend far beyond neurochemistry. This course is centered around breaking down complex research papers, which required me to assess methodology, interpret data, and evaluate conclusions. Writing blog posts and presenting information on Wednesdays forced me to distill dense material into succinct explanations—a skill that will be crucial as I pursue my doctoral studies in the fall. Discussing the science with my peers in our Wiki page presentations and in our small group discussions helped develop my ability to communication and collaboration skills. These competencies are highly transferable. In my graduate studies and beyond, the ability to analyze, synthesize, and articulate complex ideas will be invaluable.
3 & 4. Understanding Disciplinary, Interdisciplinary, and Intercultural Perspectives & Cultivating an Examined Cultural, Ethical, and Spiritual Self-Understanding
Neurochemistry doesn’t exist in a vacuum—it intersects with psychology, ethics, medicine, and even philosophy. One of the most eye-opening moments this semester was discussing the ethics of autism treatment. We didn’t just talk about the physiology of the disorder, we discussed if teachers and faculty should be required to know if students have autism. Would it perpetuate prejudice or help make sure neurodivergent students don’t fall through the cracks of the education system? We also discussed if autism needs to be cured, or if further awareness and acceptance of the disorder is the best “cure” for the disorder.
In later weeks, we discussed cultural differences that impact perceptions of anxiety when discussing adverse memory formation, and differences in cultural diets when discussing metabolic disorders. These topics forced me to think about my own morals, ethics, and actions, fostering a deeper self-awareness. This kind of interdisciplinary dialogue—between ethics, culture, science, and beyond—is a hallmark of liberal arts learning. It taught me that solving real-world problems, like improving neurological treatments, requires more than just science; it demands an awareness of societal implications.
- Encouraging Responsible Participation in the World
Perhaps the most significant takeaway from this course is that knowledge should inspire action. While I will not be entering a neuroscience-related field, I can still apply the knowledge from this course to responsibly participate in the world. Learning about various disorders allowed me to better understand how to prevent them, knowledge I can now share with my friends and family members. Most importantly, this course underscored the importance of empathy. Many disorders, from cancer to Alzheimer’s to obesity, are due to complex neurological pathophysiologies. While lifestyle choices may reduce risk, many of these disorders are multifaceted and largely out of human control. Learning about the pathogenesis of these diseases helped me to step into the shoes of those suffering and challenge any preconceived prejudices I carried to empathize at a deeper level.
A Liberal Arts Education: More Than Just a Degree
To me, learning at a liberal arts institution means breaking down barriers between disciplines. In this class, we didn’t just study neurotransmitters—we considered how they shape behavior and society. That holistic perspective is something I’ll carry forward, especially as I enter the interdisciplinary field of Industrial-Organizational Psychology.
How Neurochemistry Relates to My Future Goals: From the Classroom to Corporations
The skills and knowledge gained in neurochemistry directly support my future doctoral studies and career in Industrial-Organizational (I-O) Psychology by providing a strong scientific foundation for understanding human behavior in workplace settings. The course honed my ability to critically analyze complex systems—whether signaling pathways or organizational structures—and apply critical thinking to understand the interrelatedness of such systems. Additionally, the interdisciplinary perspective I developed, bridging neurochemistry with psychology, equips me to approach I-O challenges with unique insight. Transferable skills like oral and written scientific communication, ethical reasoning, and breaking down complex papers will be invaluable as I conduct organizational research and translate findings into practical workplace solutions. Ultimately, this course reinforced that behavior—whether in controlled lab settings or large corporate offices—is rooted in biology, neuroscience, and chemistry, an understanding that will help guide my future work.
Resume-Worthy Skill: Interdisciplinary Problem-Solving
If I had to highlight one competency I honed this semester, it would be integrating multiple perspectives to solve complex problems. At its core, neurochemistry is inherently interdisciplinary, but our discussions went beyond the fields of neuroscience and chemistry. For example, when examining neurodegeneration in Alzheimer’s disease, I considered the structure and formation of amyloid-beta plaques and tau tangles (biochemistry); possible genetic risk factors and predisposition to the disease (genetics); behavioral and cognitive consequences of Alzheimer’s (psychology); preventative strategies focusing on diet and lifestyle changes (public health); and dilemmas like early diagnosis without a cure or gene editing (ethics). This kind of multidimensional thinking is exactly what employers and graduate schools value.
Becoming Responsibly Engaged
This neurochemistry course has encapsulated my Concordia education—challenging me to think deeply, connect widely, and act thoughtfully. As I move forward, I’ll carry with me not just the MAPK pathway or the mechanics of action potentials, but also the critical, ethical, and interdisciplinary mindset that defines liberal learning.
To future students: Don’t just memorize the material—uncover how it matters in the real world. That’s what BREW is all about.


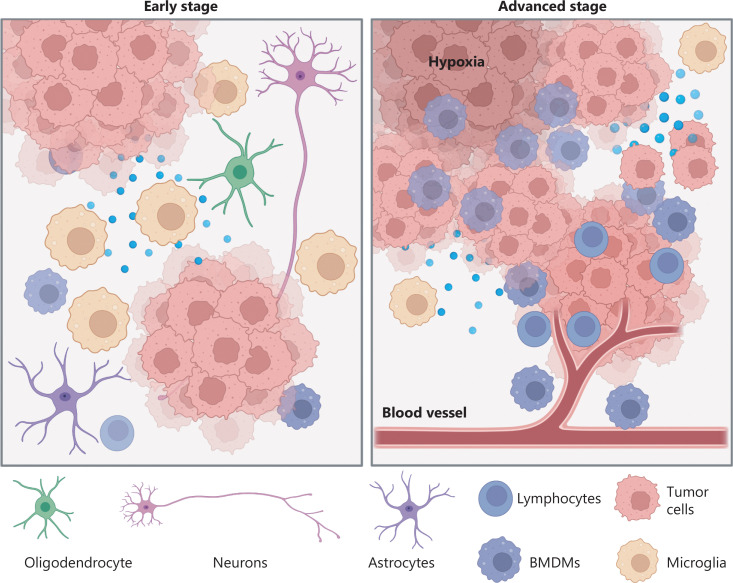
 Abstract by Alisha Debleye depicting the tumorous and dangerous growth in the human brain that can sometimes go untreated or undiagnosed.
Abstract by Alisha Debleye depicting the tumorous and dangerous growth in the human brain that can sometimes go untreated or undiagnosed.