abstract created by Gabe Sparks.
Cancer is one of the most recognized and feared diseases in our society. It has been the focus of decades of research, with countless efforts dedicated to finding a cure. Thanks to these advances, we now have a range of treatments that can successfully target many types of cancer. However, there is still much we don’t understand, and some forms of cancer continue to cause trouble for even our best therapies. While breast cancer and skin cancer are commonly known, one of the most aggressive and deadly forms often goes overlooked: glioblastoma (GBM). This malignant brain tumor is notorious for its poor survival rates, with most patients living only months after diagnosis. Despite aggressive treatment with surgery, radiation, and the chemotherapy drug temozolomide, glioblastoma remains devastatingly difficult to control.1
But new research is beginning to crack the code of how GBM survives and thrives. Potentially offering hope for smarter, more effective ways to fight back.
Understanding the Science
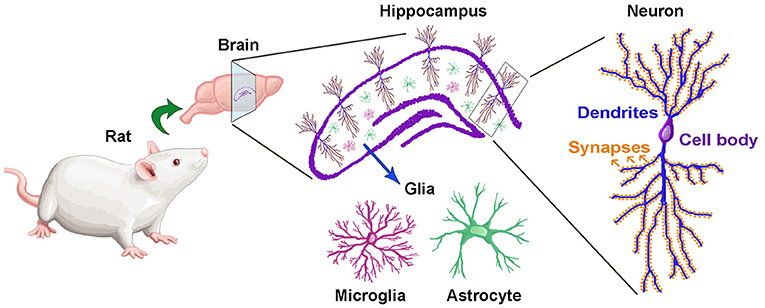
To understand the development of glioblastoma (GBM), it’s essential to look closely at three major signaling pathways: MAPK, cAMP, and PI3K. These pathways are critical for regulating key cellular functions, including metabolism, proliferation, survival, invasion, and stemness.1 Under normal conditions, they work together in a carefully balanced system to maintain healthy cell growth and tissue stability. However, when these signaling networks become disrupted or unbalanced, they can trigger uncontrolled cell growth which sets the stage for the development of GBM.
The MAPK pathway begins with the activation of a receptor tyrosine kinase (RTK) on the cell surface. Once the receptor binds its specific ligand, it triggers a cascade of intracellular events: adaptor proteins like GRB2 and SOS activate Ras, which in turn activates RAF. RAF then phosphorylates MEK, which subsequently activates MAPK. Activated MAPK moves into the nucleus, where it phosphorylates transcription factors such as CREB, leading to the recruitment of additional regulatory proteins and RNA polymerase to initiate the expression of genes that promote growth and survival.1Under normal conditions, this pathway is regulated by negative feedback mechanisms, including the tumor suppressor NF1.1 However, in GBM, NF1 is often deleted or inactivated, allowing the pathway to remain unchecked.
The PI3K pathway also starts with the activation of an RTK. Activation of PI3K leads to the conversion of PIP2 to PIP3, which then recruits and activates PDK1. PDK1 then activates AKT which is a key regulator that can translocate into the nucleus and promote gene expression that drives survival, growth, and metabolic activity.1 This pathway is normally kept in balance by PTEN (phosphatase and tensin homolog), a tumor suppressor that dephosphorylates PIP3 back to PIP2.1 In GBM, PTEN is frequently mutated, deleted, or silenced, resulting in hyperactivation of PI3K signaling.
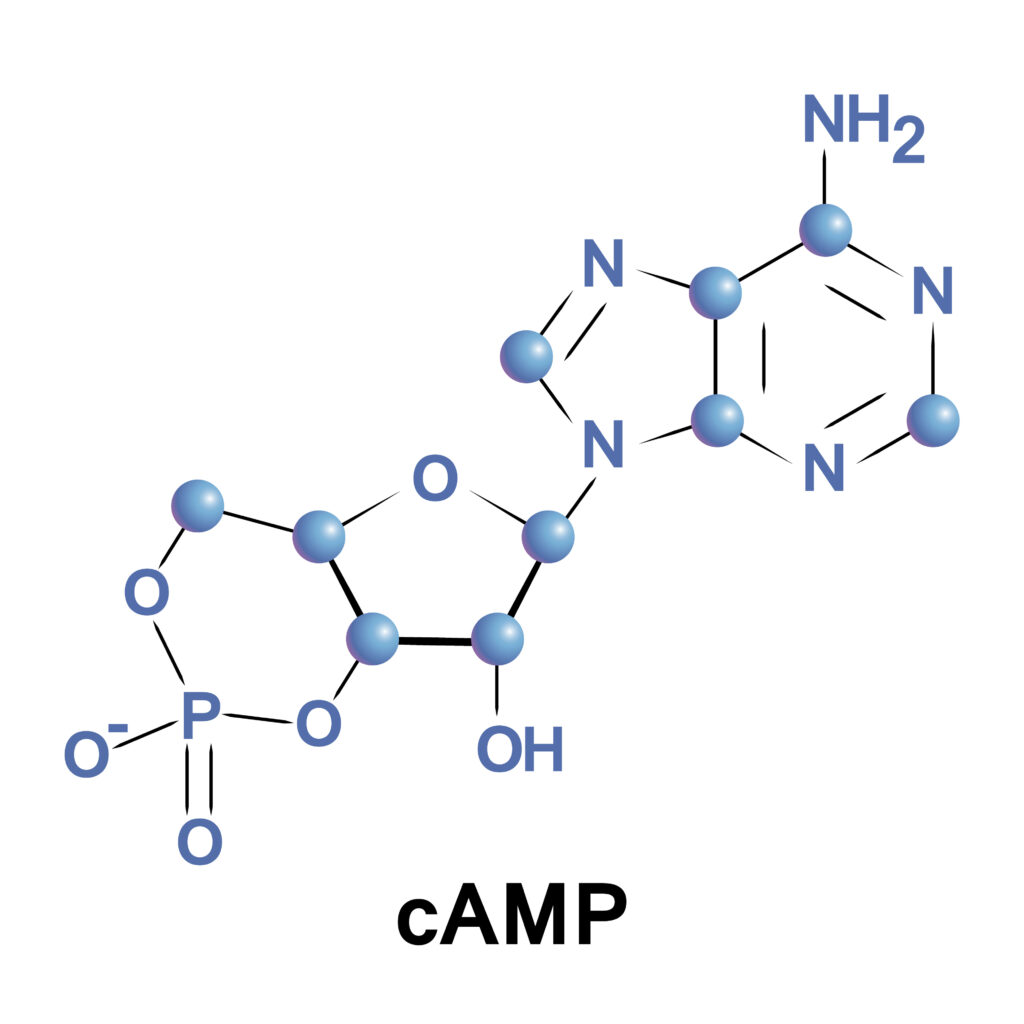
The cAMP pathway operates through a different mechanism. It begins with the binding of a ligand to a G-protein-coupled receptor (GPCR), leading to activation of adenylyl cyclase. This enzyme catalyzes the conversion of ATP to cAMP, which activates protein kinase A (PKA). PKA serves as an important modulator by inhibiting signaling at the RAF step of the MAPK pathway, thus helping to regulate cell growth. In GBM, cAMP levels are often reduced, weakening this inhibitory control and further contributing to the imbalance among pathways.
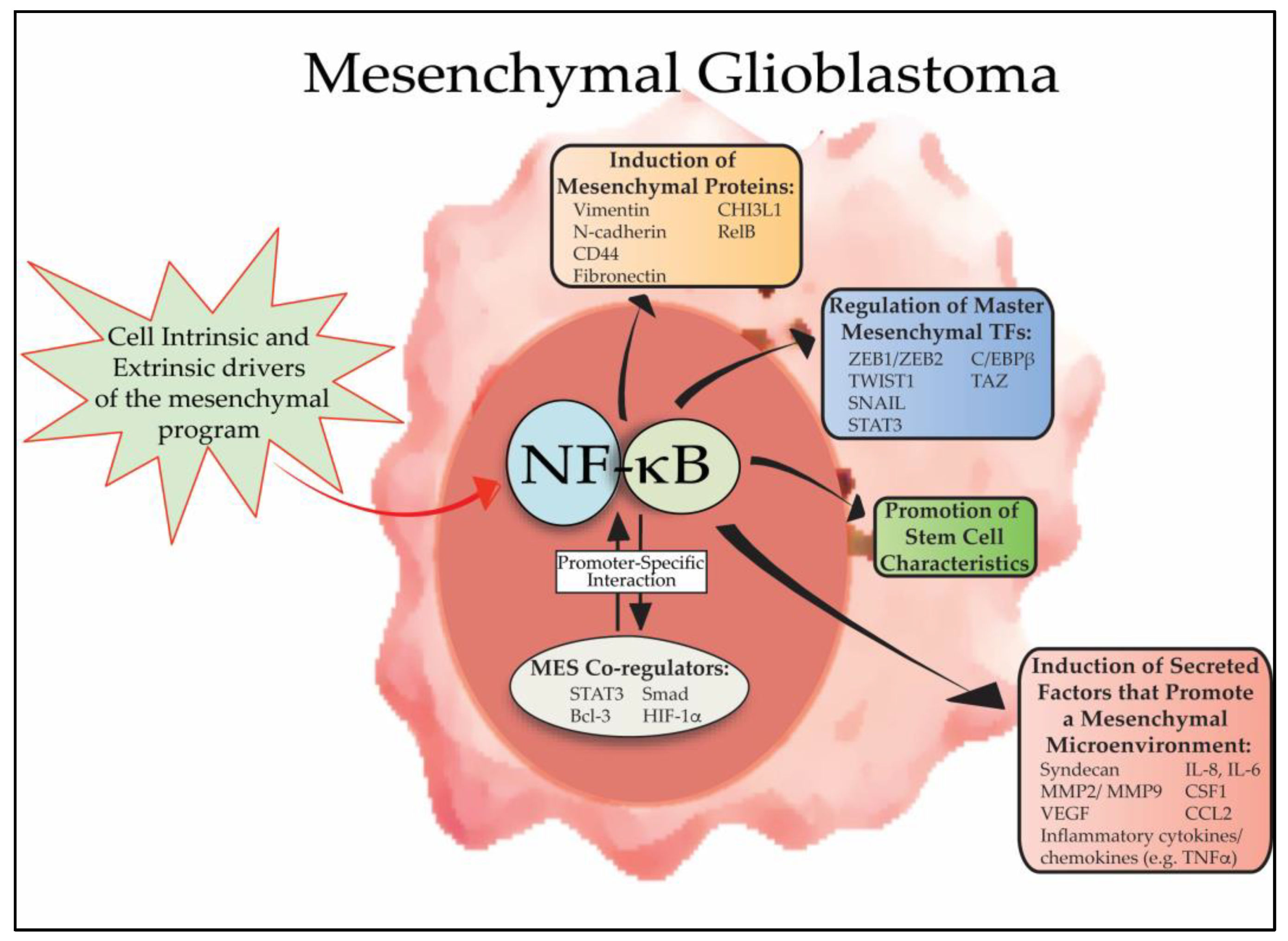
In glioblastoma, the MAPK and PI3K pathways are often hyperactivated, driving rapid and uncontrolled tumor cell proliferation, while the regulatory influence of the cAMP pathway is diminished.1 This imbalance between growth-promoting and growth-suppressing signals creates an environment where cancer cells can thrive. Figure 1 is a pictural representation of the three pathways and how they interact with one another. Here is a link to an article that goes into great detail on how these pathways play a role in GBM.

Figure 1. Pictorial representation of the multiple pathways involved in GBM.
Fortunately, recent advances in research are uncovering new strategies to target these disrupted signaling networks and bring new hope in the fight against GBM.
Emerging Treatments
Despite the major challenges presented by glioblastoma’s complexity and resistance to treatment, several promising new therapies are under active investigation. One major area of focus is immunotherapy, which aims to help the body’s own immune system recognize and attack tumor cells. Immune checkpoint inhibitors that target proteins like PD-1, PD-L1,and CTLA-4 are being tested, often in combination, to boost immune activation against GBM.2 Another exciting strategy is CAR T-cell therapy, where a patient’s T cells are genetically engineered to recognize specific tumor markers such as EGFRvIII and IL13Rα2.2 While these approaches show great promise, challenges like tumor relapse and immune evasion remain, highlighting the need for further investigation.
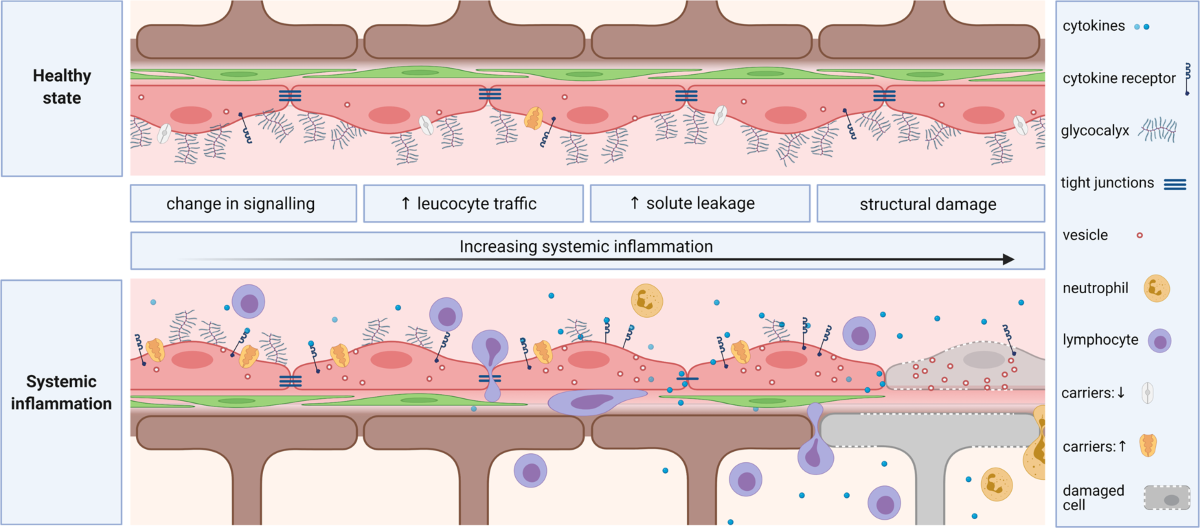
Nanocarrier-mediated therapy is another cutting-edge field. Researchers are developing nanoparticles designed to cross the blood-brain barrier and deliver drugs directly to tumor cells.2 By targeting cancer cells more precisely, these nanocarriers hope to improve treatment effectiveness while minimizing side effects. Magnetic nanoparticles, in particular, are entering clinical trials and may offer a new solution for delivering therapies deep within the brain.2
While many of these new therapies are still in early stages of development, they are already showing encouraging results. Together, they represent an exciting shift in how we approach one of the most challenging cancers. Here is a link to an article that explores many of the new treatments being developed.
Conclusions
GBM is a devastating form of cancer that too often goes overlooked. While more common cancers like breast and skin cancer receive widespread attention, it’s crucial that we shine a light on all forms of cancer especially those as aggressive and lethal as GBM. Increasing public awareness can drive not only a deeper understanding of this disease but also greater support for the research needed to develop new, life-saving treatments. By broadening the conversation around cancer, we can help accelerate progress and offer hope to those affected by glioblastoma and other under-recognized cancers.
References
(1) Fung, N. H.; Grima, C. A.; Widodo, S. S.; Kaye, A. H.; Whitehead, C. A.; Stylli, S. S.; Mantamadiotis, T. Understanding and Exploiting Cell Signalling Convergence Nodes and Pathway Cross-Talk in Malignant Brain Cancer. Cellular Signalling. Elsevier Inc. May 1, 2019, pp 2–9. https://doi.org/10.1016/j.cellsig.2019.01.011.
(2) Angom, R. S.; Nakka, N. M. R.; Bhattacharya, S. Advances in Glioblastoma Therapy: An Update on Current Approaches. Brain Sciences. Multidisciplinary Digital Publishing Institute (MDPI) November 1, 2023. https://doi.org/10.3390/brainsci13111536.