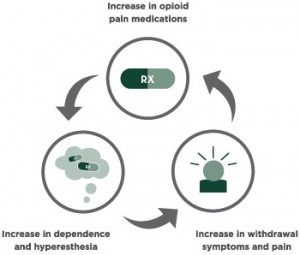
Addiction is defined as having a craving or dependence to a substance, thing, or activity. Addiction can be tied to a natural reward such as sleep, food, etc. whereas it can also be tied to an unnatural reward such as substances. Unnatural addictions such as drugs or alcohol can be life threatening at times and turn into a horrific cycling pattern if trying to withdraw and stop usage.
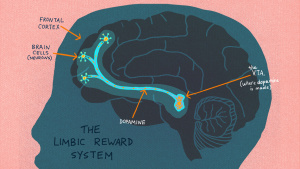
In the brain there are three areas of the brain an addiction behavior can go through:
- The first is the basal ganglia, the portion of the brain that controls the reward response to the substance use and helps to form the habits around substance use.
- The second is the extended amygdala that associates with the feelings of discomfort, anxiety, stress that usually follows substance withdrawal.
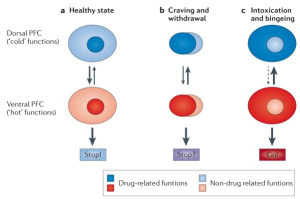
- The third is the prefrontal cortex which controls the ability to have control over the substance usage.
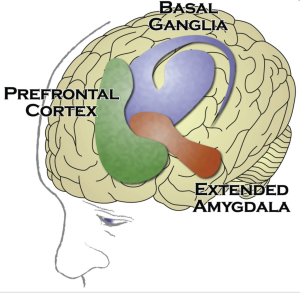
Figure 1: The different areas of the brain affected by addiction. https://www.ncbi.nlm.nih.gov/books/NBK424849/
The overwhelming effects of addiction occurs when this cycle repeats itself and the addiction grows stronger after making those rewarding affects attainable with the substance rather than without.
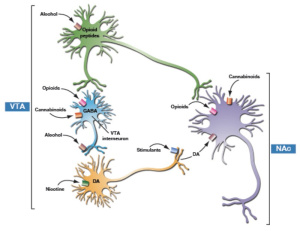
Studies suggest that individuals with an addiction to substances have a reduction in sensitivity for the brain’s reward system (brain circuits with dopamine receptors). Therefore, once pleasurable or stimulating activities no longer have the same effect as they once did, an individual going through withdrawal symptoms will want to regain the same pleasurable feelings the reward system once provided but only be able to do this through the substance.
At the more neuronal level, during the withdrawal stage there is an activation of the stress neurotransmitters in the extended amygdala. These NTs include corticotrophin-releasing factor (CRF), norepinephrine, and dynorphin. These neurotransmitters have been shown to play a key role in negative feelings associated with withdrawal. Therefore, to get rid of the negative emotions from withdrawal a lot of individuals tend to use the substance again. In other words, the individual is experiencing negative reinforcement every time they use the substance again to rid themselves of the negative emotions and this is how the cycle continues.
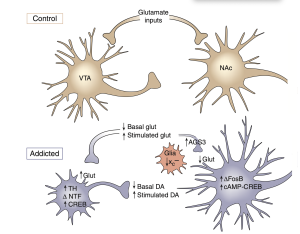
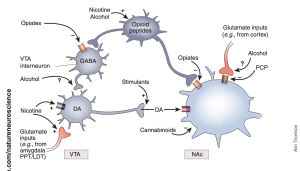
Taking a closer look at the brain it is important to understand the difference between an addicted brain versus an unaddicted brain to a substance. In the control brain, VTA dopaminergic neurons project to NAc whereas with the addicted brain neurons there is an increase of dopamine in NAc (Nucleus accumbens) leading to tolerance, sensitization, and adaptation to the substance. In the addicted brain, the VTA neuron appears smaller as the NAc portion is larger in size with more branching, leading to the effects of becoming addicted to a substance and unable to stop.
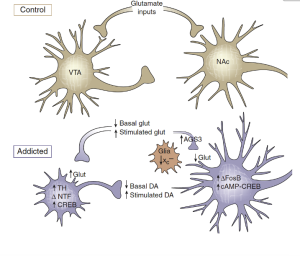
Figure 2: Image of neurons in the brain from Nestler article (2005).
Overall, addiction starts as a choice and turns into a gray area where the choice of using a substance is no longer there. As there has been some controversy on whether addiction is a disease, in the future when we learn more about addiction and what more is happening in the brain can we decipher if the individual has a choice or if that choice is no longer there once the brain creates tolerance, sensitization, and adaptation to the substance.
References:
Substance Abuse and Mental Health Services Administration (US), Office of the Surgeon General (US), and US Department of Health and Human Services. 2016. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK424849/
Nestler, Eric. 2005. Is there a common molecular pathway for addiction? Nature Neuroscience: Neurobiology of Addiction.
Leyton, Marco. 2013. Are addictions diseases or choices? Journal of Psychiatry & Neuroscience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3692718/









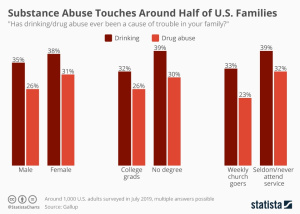 Statistically,
Statistically, 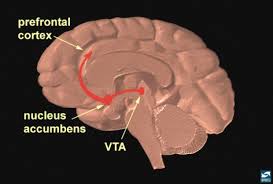 Addicts will choose this feeling over anything else in their life because eventually their brains don’t feel motivation or reward for any other activity other than using their drug of choice. Even with their drug of choice, they will eventually need to increase the amount they take to keep that high.
Addicts will choose this feeling over anything else in their life because eventually their brains don’t feel motivation or reward for any other activity other than using their drug of choice. Even with their drug of choice, they will eventually need to increase the amount they take to keep that high.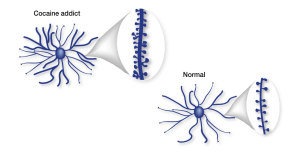 Part of the brain responsible for reason, judgment, learning, and memory begin to have changes as well. In some spots, the neurons are pruned back whereas in other regions there are more connections, completely changing the shape of the neuron. After all of these changes, the drug-seeking behavior becomes habit and the person becomes addicted.
Part of the brain responsible for reason, judgment, learning, and memory begin to have changes as well. In some spots, the neurons are pruned back whereas in other regions there are more connections, completely changing the shape of the neuron. After all of these changes, the drug-seeking behavior becomes habit and the person becomes addicted. Relapse is defined as when a person returns to using drugs or alcohol after a period of sobriety. There are many factors that contribute to relapsing, which can be seen in this image. After the neurons are changed and the feeling and memories of drugs are implanted into someones brain it can be extremely hard to just give it up. The brain is still searching for this increased reward feeling and it isn’t getting it from ‘normal’ daily activities which can make turning back to drugs really tempting.
Relapse is defined as when a person returns to using drugs or alcohol after a period of sobriety. There are many factors that contribute to relapsing, which can be seen in this image. After the neurons are changed and the feeling and memories of drugs are implanted into someones brain it can be extremely hard to just give it up. The brain is still searching for this increased reward feeling and it isn’t getting it from ‘normal’ daily activities which can make turning back to drugs really tempting.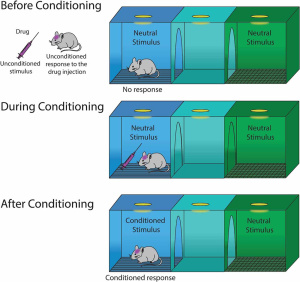 Conditioning is defined as a higher dose of drugs that can be tolerated when external stimuli is associated with prior administration of the drug is present. Basically, this means that if someone is doing drugs in the same room at the same time everyday they will eventually build up a tolerance because their brain will release the the effects of the drug before it is even taken. This leads to a tolerance, and if the drug is taken with any of the external factors changed it can lead to an overdose.
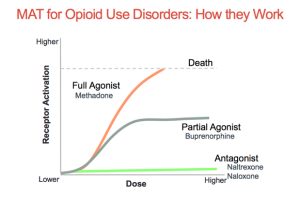
Conditioning is defined as a higher dose of drugs that can be tolerated when external stimuli is associated with prior administration of the drug is present. Basically, this means that if someone is doing drugs in the same room at the same time everyday they will eventually build up a tolerance because their brain will release the the effects of the drug before it is even taken. This leads to a tolerance, and if the drug is taken with any of the external factors changed it can lead to an overdose. Recovery is much more complex than it is made out to be. There are many factors that play a part in the life of an addict. It is not as simple as quitting cold turkey sometimes. There are memories and outside factors that can effect the ability to remain sober. Being educated on all the facts of addiction can help stop the stigma that it is just a simple choice. It truly goes down to the cellular and molecular level and changes are happening at those levels making it difficult to change behaviors right away. Treatment for addiction can be very expensive and difficult.
Recovery is much more complex than it is made out to be. There are many factors that play a part in the life of an addict. It is not as simple as quitting cold turkey sometimes. There are memories and outside factors that can effect the ability to remain sober. Being educated on all the facts of addiction can help stop the stigma that it is just a simple choice. It truly goes down to the cellular and molecular level and changes are happening at those levels making it difficult to change behaviors right away. Treatment for addiction can be very expensive and difficult.