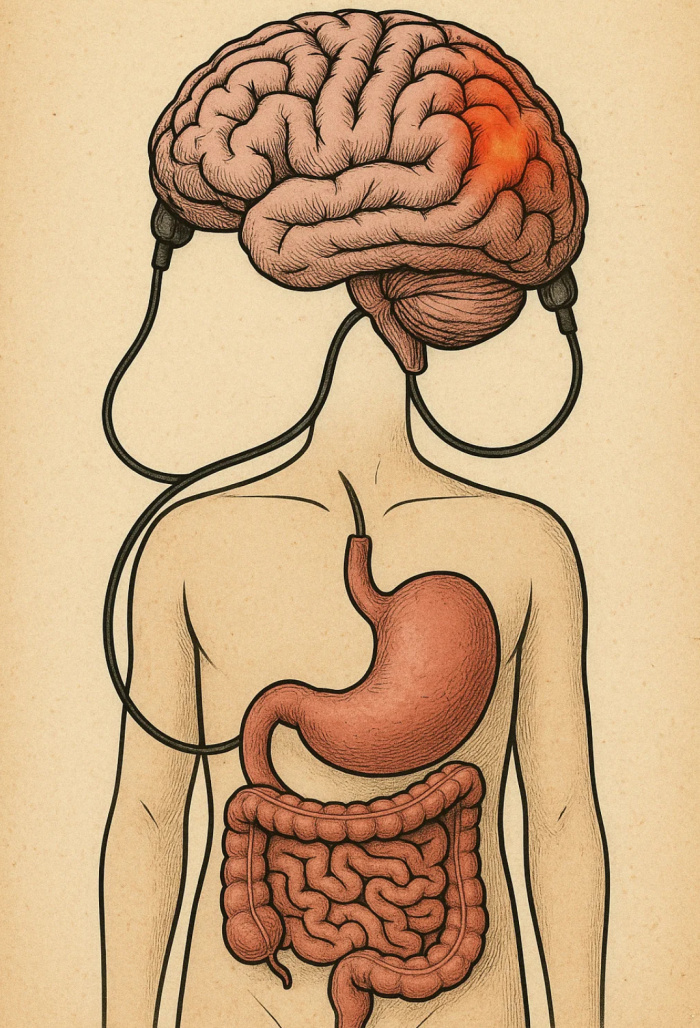
Cannabis has captivated human attention for centuries, from ancient herbal remedies to its modern role as a controversial therapy. But beyond the cultural conversation, modern science has pulled back the curtain to reveal a fascinating biological system deeply woven into the human body: the endocannabinoid system (ECS). Understanding this system—especially the cannabinoid receptors CB1 and CB2—is key to unlocking cannabis’s full therapeutic potential.
What Is the Endocannabinoid System (ECS)?
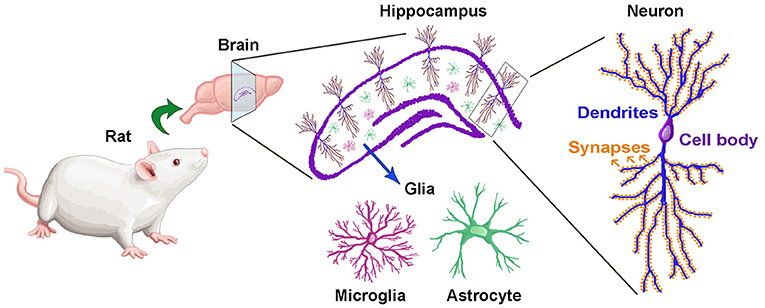
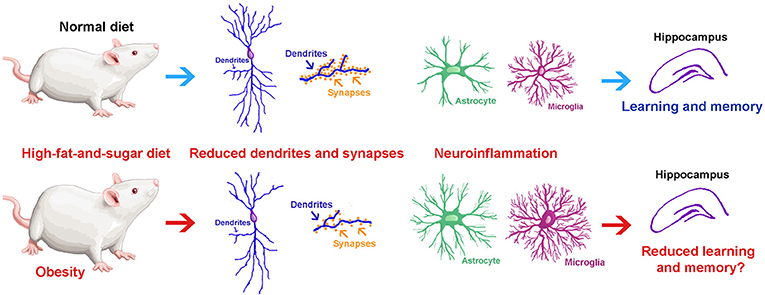
The ECS is a vast and complex network within our bodies that helps regulate vital functions like synaptic plasticity, homeostasis, pain perception, memory, mood, and even immune responses. At the heart of this system are two major players: CB1 and CB2 receptors.
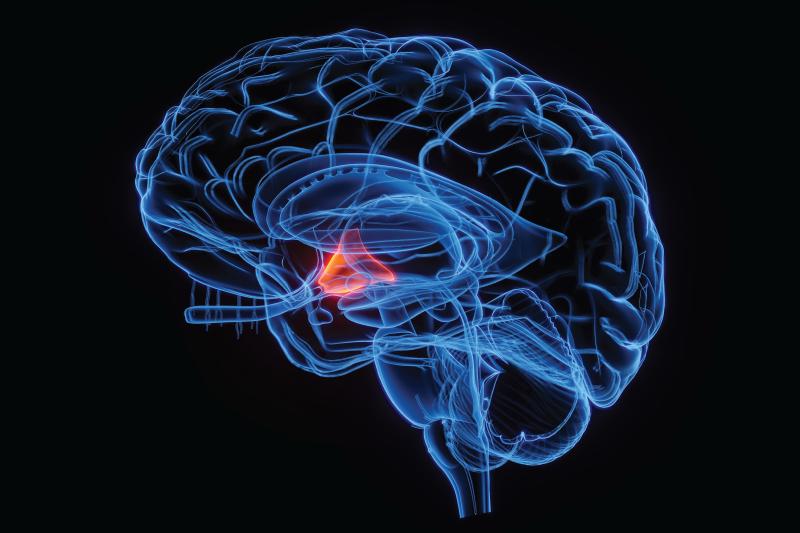
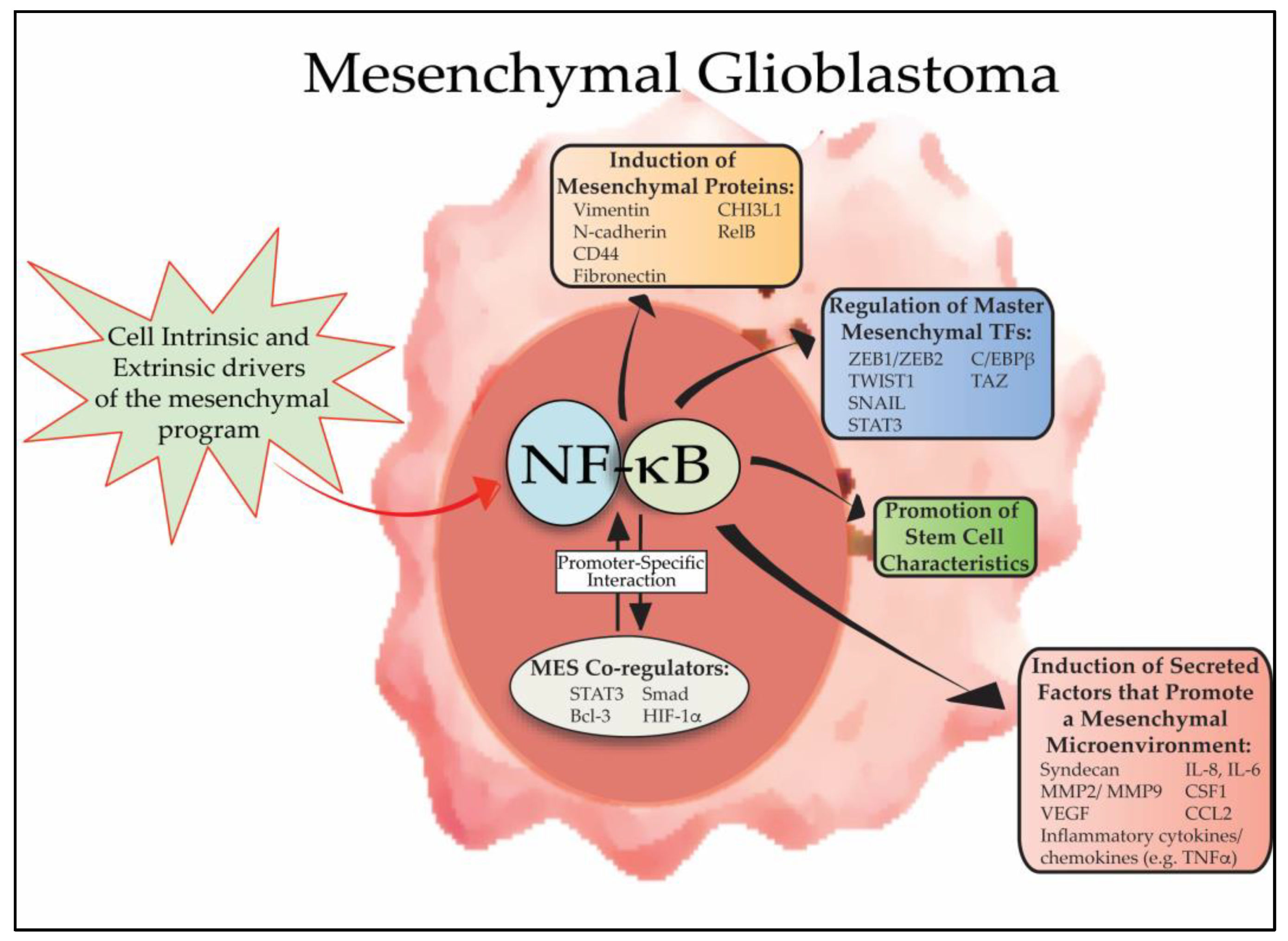
- CB1 receptors are mostly found in the central nervous system (CNS). These receptors are responsible for the majority of psychoactive effects associated with cannabis, especially those triggered by THC (tetrahydrocannabinol). They influence the release of neurotransmitters, modulate synaptic activity, and play key roles in memory formation, mood regulation, and motor control.
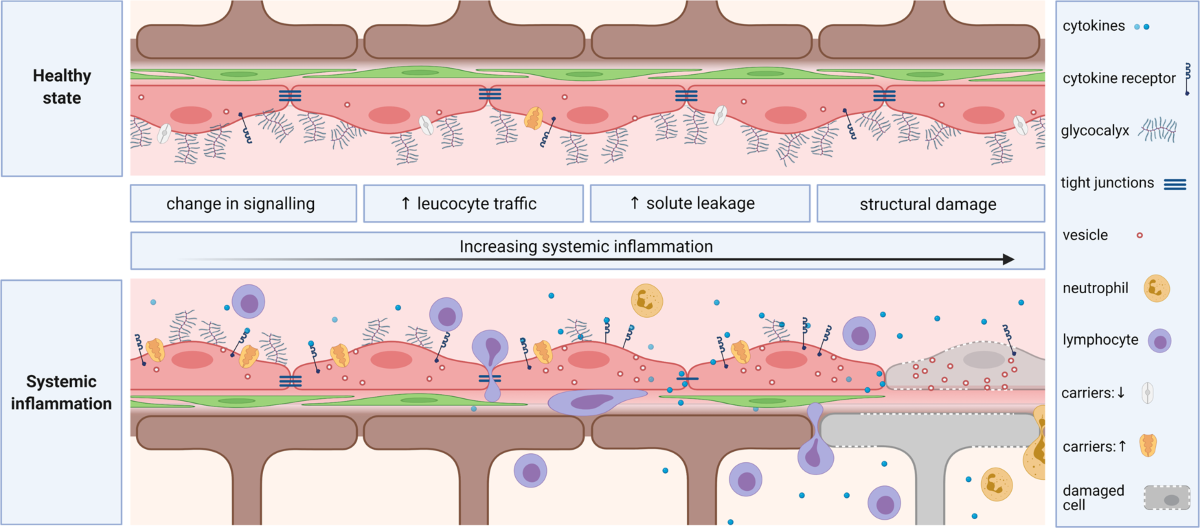
- CB2 receptors, on the other hand, are typically associated with immune cells, though they also appear in the CNS, particularly during times of injury or disease. These receptors contribute to regulating inflammation and may provide neuroprotection in conditions like multiple sclerosis and Alzheimer’s disease.
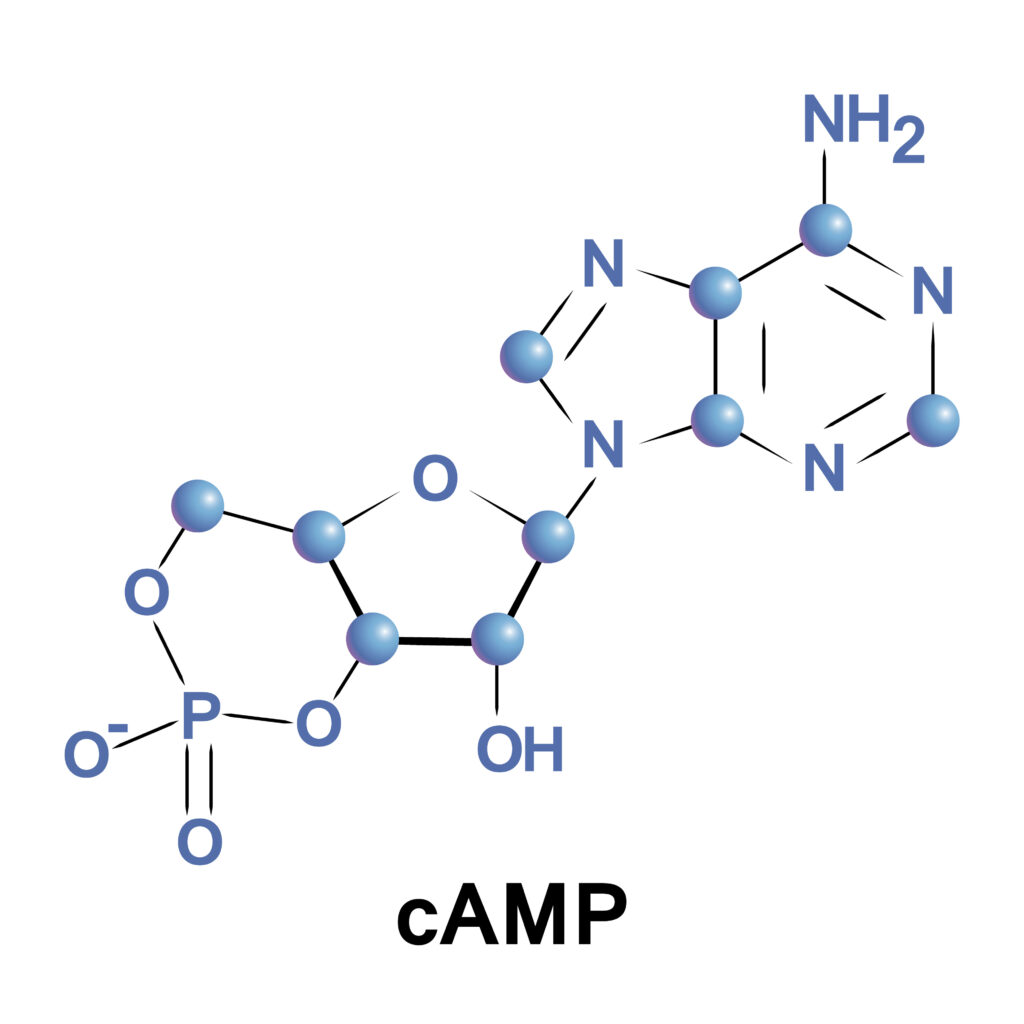
Our bodies produce their own “natural cannabis-like chemicals,” called endocannabinoids, such as anandamide (AEA) and 2-arachidonoylglycerol (2-AG). These molecules help fine-tune communication between cells, ensuring that our nervous and immune systems remain balanced. [1]

This figure depicts the cell signaling mediated by CB1 receptor activation. [2]
Cannabis, Disease, and the ECS
Research has shown that dysregulation of the ECS is associated with several neurological and autoimmune conditions:
- In Alzheimer’s disease, CB1 receptor activity may offer neuroprotection by limiting inflammation and neuron death.
- In Huntington’s disease, alterations in CB1 receptor signaling are thought to contribute to disease progression.
- Multiple sclerosis (MS) patients may benefit from cannabinoid-based therapies that reduce spasticity and pain.
- After a traumatic brain injury (TBI), endocannabinoid signaling often ramps up, which may help the brain cope with trauma.
Importantly, endocannabinoid signaling is tightly linked with intracellular calcium levels and synaptic plasticity, suggesting that targeting this system could have far-reaching implications for treating both chronic pain and mental health conditions. [1]
Pharmaceutical Advances: Sativex and Beyond
One of the most promising examples of cannabis-based therapy is Sativex, an oromucosal spray containing a roughly 1:1 ratio of THC and CBD (cannabidiol).
Key points about Sativex:
- It’s primarily used for neuropathic pain, spasticity in MS, and opioid-resistant pain.
- It mimics the body’s own natural pain-relieving mechanisms.
- It shows mild physiological effects like slight heart rate increases and occasional anxiety, but no major adverse events.
- Compared to smoked cannabis, it provides slower absorption and delayed onset (3–6 hours), allowing patients better control over dosing and minimizing the risk of severe psychoactive side effects.
Clinical relevance: Sativex represents a major step forward—offering a safer, controlled, and standardized way for patients to benefit from cannabinoids without many of the risks associated with traditional cannabis use. [3]
Ethics and the Future of Cannabinoid Research
As scientific curiosity around cannabis grows, an important question looms: Should we keep investing in cannabinoid research?
From a medical standpoint, the answer seems clear—yes. The ECS regulates many critical systems in the body, and deeper insights could lead to treatments for devastating illnesses like Alzheimer’s, multiple sclerosis, chronic pain, epilepsy, and even cancer. The possibilities for neuroprotection, immune modulation, and pain management are too great to ignore.
However, there are ethical considerations:
- Risk of misuse: As cannabis-based treatments become more available, there is a danger of blurred lines between therapeutic use and recreational abuse, especially among vulnerable populations.
- Access and equity: Will cannabis-based therapies be accessible to all patients, or will they be priced out of reach?
- Long-term effects: We still don’t fully understand the long-term impact of chronic cannabinoid use, particularly on developing brains.
- Stigma: The historical stigma surrounding cannabis could discourage both patients and doctors from exploring legitimate treatments.
Despite these challenges, the potential benefits outweigh the risks—especially when research is conducted thoughtfully, ethically, and with a focus on scientific rigor and patient well-being.
Conclusion
Cannabis is much more than a cultural phenomenon—it is a doorway into one of the body’s most fascinating regulatory systems. By unlocking the secrets of the endocannabinoid system, researchers are paving the way for safer, smarter therapies that could transform how we treat some of the most challenging diseases known to humankind.
The future of medicine may very well be green—but only if we continue the work with open minds, cautious hands, and a commitment to scientific excellence.
To learn more about this topic click here.
[1] D. A. Kendall and G. A. Yudowski, “Cannabinoid Receptors in the Central Nervous System: Their Signaling and Roles in Disease,” Front. Cell. Neurosci., vol. 10, Jan. 2017, doi: 10.3389/fncel.2016.00294.
[2] L. Tian et al., “Cannabinoid receptor 1 ligands: Biased signaling mechanisms driving functionally selective drug discovery,” Pharmacology & Therapeutics, vol. 267, p. 108795, Mar. 2025, doi: 10.1016/j.pharmthera.2025.108795.
[3] E. L. Karschner et al., “Subjective and physiological effects after controlled Sativex and oral THC administration,” Clin Pharmacol Ther, vol. 89, no. 3, pp. 400–407, Mar. 2011, doi: 10.1038/clpt.2010.318.