Should I care about Alzheimer’s? Yeah probably….
Artstract by: Alex Braun
Protein basics
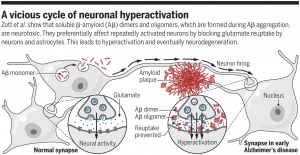
To understand how to help prevent yourself from developing Alzheimer’s disease, it helps to have some background information about the disease. Alzheimer’s disease is thought to be caused by the abnormal buildup of proteins in and around the brain cells. One of these proteins is amyloid, deposits of which form plaques around brain cells. The other protein, tau, deposits of which form tangles in the brain cells (NHS et al., 2021).
Amyloid Plaques
Amyloid is a protein fragment that the body produces naturally. Amyloid plaques are hard, insoluble accumulations of beta amyloid proteins that clump together between the neurons. The reason these plaques are hard to dissolve in the fluid between cells is because the enzyme that cuts the amyloid precursor protein (APP), cuts strands that are too large. Since these strands are too large, they are “sticky” and start clumping into deposits which are referred to as plaques (BrightFocus et al., 2020).
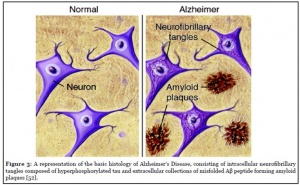
Neurofibrillary tangles
Neurofibrillary tangles are insoluble twist fibers primarily consisting of the protein, tau. These tangles form when tau is misfolded in a peculiar way. Specifically, in Alzheimer’s disease, tau forms a C-shape in the core in the core of the tangle with a loose end sticking out randomly. Once a tangle has been started, more tau proteins are recruited to make it longer (BrightFocus et al., 2020).
This all sounds scary, so how can one help prevent developing Alzheimer’s disease
Well, it’s not exactly as simple as just “do this and you won’t get Alzheimer’s” because life would be too easy if that was the case. You can however, live a healthy lifestyle and keep an active brain to help reduce your chances of developing Alzheimer’s disease
Cardiovascular and Alzheimer’s
Cardiovascular disease has been linked with an increased risk of Alzheimer’s disease. You can reduce your risk of developing both cardiovascular disease and Alzheimer’s disease by not smoking, drinking alcohol in moderation, eating a balanced diet, and exercising (NHS et al., 2021). I know this sounds redundant to say, but seriously, just live healthy and you’ll be better off.
Staying mentally active
There’s some evidence to suggest that rates of dementia are lower in people who remain mentally and socially active throughout their lives. One may be able to reduce their risk of Alzheimer’s disease by reading a book, learning a new language, playing an instrument, group sports, being social (NHS et al., 2021) One could also play “brain training” computer games which haven’t been fully proven to prevent Alzheimer’s, but who knows, you might even have some fun.
Other factors
Factors that are not directly responsible for Alzheimer’s disease but play a role in development include hearing loss, untreated depression, and loneliness (NHS et al., 2021) So, if you know someone who is lonely or depressed, go be their friend so you can help them reduce their risk of developing Alzheimer’s.
Works cited
Amyloid plaques and neurofibrillary tangles. BrightFocus Foundation. (2020, March 13). Retrieved from https://www.brightfocus.org/alzheimers-disease/infographic/amyloid-plaques-and-neurofibrillary-tangles.
NHS. (2021, July 5). Causes of Alzheimer’s Disease. NHS choices. Retrieved from https://www.nhs.uk/conditions/alzheimers-disease/causes/.
Signaling in the Brain is The Tightest Regulation Around
Have you ever felt like you are following too many rules in your life, or that you have too little control in major life events? This phenomenon is all too common, but in the brain specifically it takes regulation and rules to a whole new level. In the brain it is dangerous to have both too much or too little of many chemicals and proteins, so much so that diseases such as Alzheimer’s disease can be cause both by too much or too little of certain chemicals that our brain depends on for normal function.
What is Grb and What Does it Do?
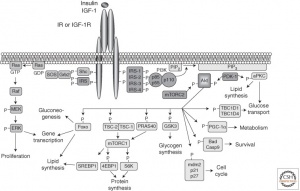
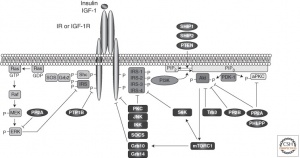
Grb is one of many vital proteins in the brain, and it is part of the MAPK pathway. This pathway is one of the most tightly regulated pathways due to its ability to both help and inhibits the usage of insulin in our brains. There are two separate mechanisms of insulin: regular insulin signaling and the competition against insulin, where MAPK performs exactly the same function in two different environments.
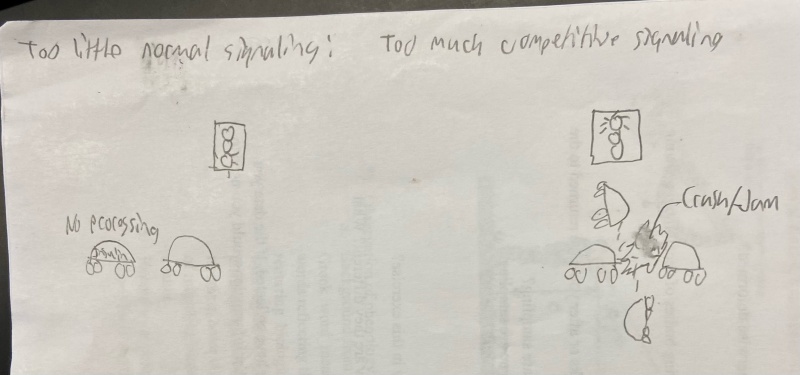
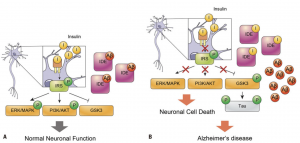
Breaking down the two pathways; too little normal signaling can be compared to a traffic stop where the light is green and there is a car not proceeding. When that car is not moving, the entire normal pathway is slowed and insulin can’t perform its vital functions in the brain. On the other hand, when the competitive insulin pathway is overstimulated, the situation is similar to a traffic junction where a car blows a red light and starts to cause a traffic jam in the intersection. In this case, too many “cars” in the signal pathway causes a blockage that prevents insulin from doing its job in the brain. Notice how in the two images below the left pathway (MAPK) never changes, but the end result is two entirely different impacts on the insulin binding site. More on Grb and these pathways
Why is this blockage bad?
When insulin is blocked in the brain, there is a wide host of problems that can occur, one of those many problems is the beginnings of Alzheimer’s disease. Many studies have linked Alzheimer’s disease to the inability to properly regulate insulin. Due to the above pathway obstructions (both too little normal signaling and too much competition), insulin will build up and cause a hyperglycemia in the brain. This buildup of sugar leads to the two telltale signs of Alzheimer’s disease; amyloid beta plaques outside the neurons and phosphorylation of a dangerous tau protein inside the cells. These work together to cause irreparable damage to the brain, specifically the neurons that help transmit information. Individuals infected with Alzheimer’s see a substantial drop in their cognitive function, which leads to major quality of life impacts. Once this destructive pathway becomes active, there isn’t much we can do to stop it with current technology outside of treating the symptoms and placing the individuals under the care of another person as their own capacities begin to fail. This demonstrates how important it is to follow the rules and regulations of the brain, even if you don’t necessarily follow all the rules outside the brain. More on insulin and Alzheimer’s Diesase
Exploring the Caspase Family in Alzheimer’s Disease
An Overview of Alzheimer’s Disease:
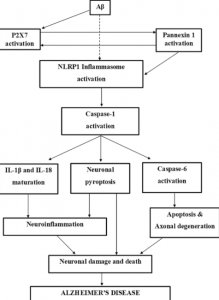
Alzheimer’s Disease (AD) is a neurodegenerative disease characterized by progressively worsening executive cognitive functioning, including memory impairment and overall cognitive deficits. The symptoms start small and may not even be noticed but for the following years, the disease will become much more apparent. Hyperphosphorylation of the tau protein causes the production of neurofibrillary tangles and amyloid-beta plaques, which trigger neuroinflammatory pathways, eventually leading to neurodegeneration/apoptosis, decreasing brain size. 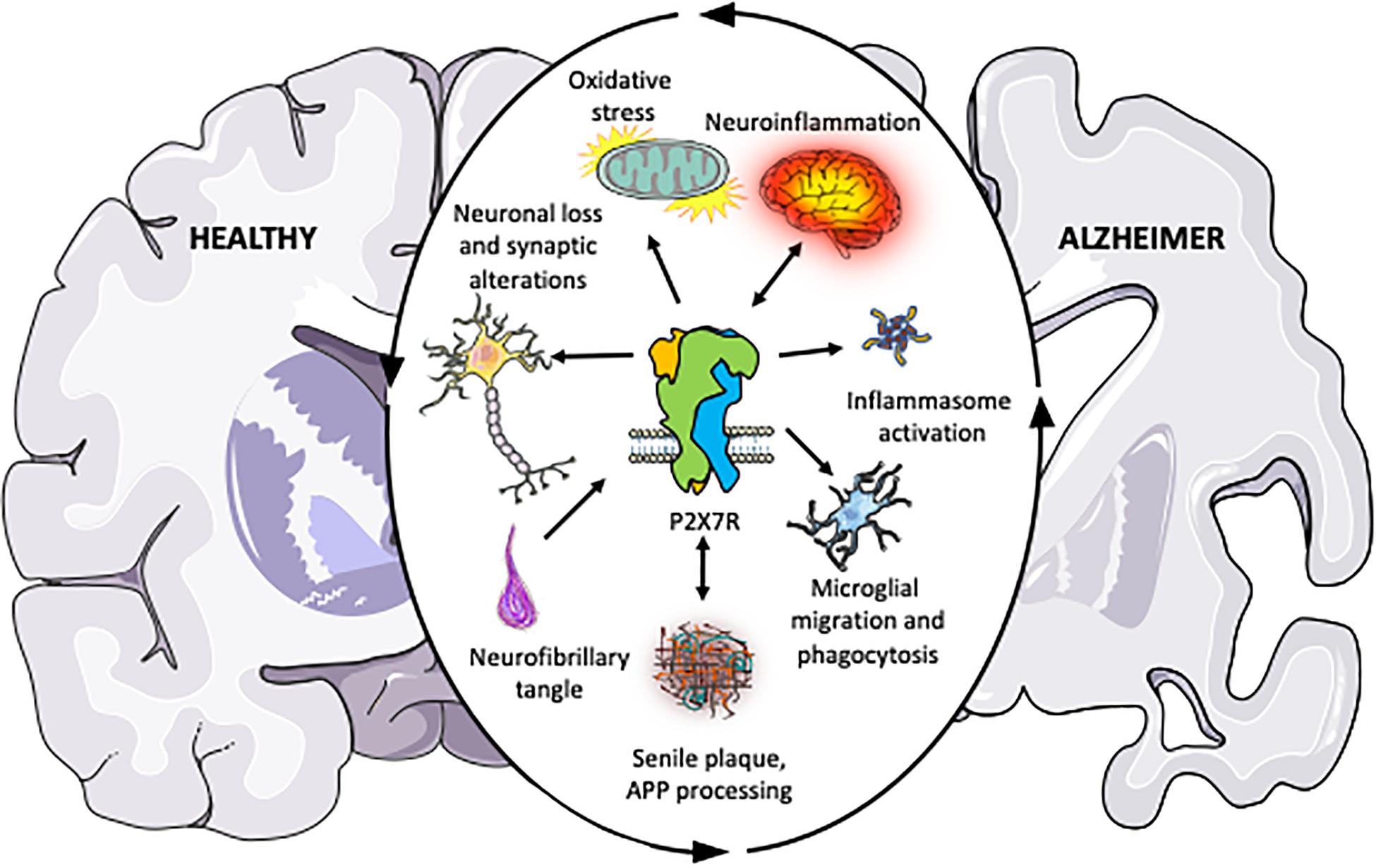
The Caspase Family:
The caspase family includes caspase 1-12 and are all protease enzymes that play significant roles in neuroinflammatory and pro-apoptotic processes. As proteases, these enzymes (caspase 3, 6, and 7) break down proteins into peptide chains, then further into individual amino acids.
The inflammatory caspases (1, 4, 5, 8, and 11) initiate the inflammatory response after a pro-inflammatory cytokine binds to the corresponding receptor. Different caspases communicate with each other to transduce the cytokine’s signal to the cell nucleus, where pro-inflammatory gene transcription is upregulated, leading to higher degrees of cell inflammation. In terms of AD, inflammatory caspases can aggravate the neurofibrillary tangles and amyloid plaques, which can trigger neurodegenerative processes, eventually leading to apoptosis. 
Crystal structure of Caspase-3 (3DEI), the caspase gaining most attention as a possible therapeutic target
The pro-apoptotic and neurodegenerative caspases (2, 8, 9, and 10) are responsible for initiating the apoptotic pathway, leading to the breakdown of various proteins inside the cell into peptides and amino acids, which can lead to the neuron or cell becoming nonfunctional, which triggers programmed cell death pathways. This explains why post-mortem analyses of AD brains are significantly smaller in size than non-AD brains.
The figure below illustrates this idea of how NFT/AB plaques, neuroinflammation, and neurodegeneration are all related through the caspase proteases. https://pubmed.ncbi.nlm.nih.gov/31111399/
Apoptosis and Neurodegeneration:
It is important to note that caspase-mediated neuroinflammatory and neurodegenerative pathways are not themselves impaired in AD progression. Caspases do not like neurofibrillary tangles or amyloid plaques. Their interaction stimulates cytokine release and the pathway that follows responds the way it is supposed to. These proteases are behaving exactly the way they are meant to, but the dysfunction of the upstream pathways is constantly triggering these events.
Can we Treat AD with Caspase Inhibitors?
The short answer is yes, but it may not be a very effective therapeutic aspect in terms of “curing” Alzheimer’s. The formation of neurofibrillary tangles and amyloid-beta plaques is a required prerequisite for hyperstimulating pro-inflammatory cytokine release and thus neurodegeneration and apoptosis. These steps are consequences far downstream from severe kinase pathway dysfunction and developing successful caspase-targeted drugs would not do anything to stop or retard the progression of the disease.
Caspases are at the end of the signal transduction pathway. The progression of AD is not a simple, one-road track. This disease is caused by severe dysfunction of nearly every protein involved in an already complex signal transduction pathway. The caspases are far downstream from these proteins and their actions are a result of chaotic impairment of upstream functioning. Developing a caspase inhibitor could marginally increase the cell lifespan, but in terms of AD pathogenesis, it would do nothing to prevent the disease from progressing. This paper goes further into the neurochemistry of caspase-mediated apoptosis in AD and explains caspase-targeted drug outlook more in-depth. https://pubmed.ncbi.nlm.nih.gov/11556539/
Summary
Caspases are largely responsible for inflammation, neurodegeneration, and apoptosis in Alzheimer’s Disease. While their specific pathways are not dysfunctional themselves, their activity is a result of dysfunction throughout upstream pathways that lead to tau hyperphosphorylation. As proteases that are towards the end of the AD-progressing pathway, using them as drug targets could prolong cell life and may increase cell lifespan at best, but the progression of the disease is much more complicated.
Lifestyle factors can impact brain health
Alzheimer’s disease:
New research keeps shedding light on Alzheimer’s Disease prevention and treatment. New studies have linked Diabetes Mellitus Type II, which is a major disease in the United States, as a major factor that can contribute to someone developing Alzheimer’s Disease in the future. Insulin functioning in Alzheimer’s Disease is a major topic that is being explored. https://www.sciencedirect.com/science/article/abs/pii/S019701862030098X?via%3Dihub
What is insulin?
Insulin is a hormone that is released by the body after food is eaten to lower blood sugar. Insulin helps to lower blood sugar by activating cells to store sugar in a long chain, called glycogen, which can be used as a fuel reserve as a gas tank is a fuel reserve for a car.
Variations in diet, even genetics, can change how much insulin needs to be produced by the body. Diets high in sugar and saturated fats, think of fats that are solid at room temperature like coconut oil, can increase insulin production. Eating diets that are high in sugar and saturated fats for many, many years, can increase the likelihood of developing insulin resistance as seen in Figure 1.
What is insulin resistance?
Insulin resistance essentially means that the cells of the body are no longer being activated to the same capacity because the cells have gotten used to so much insulin. Think of this as putting a phone on energy saving mode compared to never putting the phone on energy saving mode, the phone screen is not as bright, the screen turns black faster when not being used, and does not function as usual.
Developing insulin resistance can be increased from having an excess amount of body fat, which can result in obesity. Severe insulin resistance can be diagnosed as Diabetes Mellitus Type II. https://www.diabetes.org/healthy-living/medication-treatments/insulin-resistance
Insulin resistance and Alzheimer’s disease
Developing Type II Diabetes reduces the effectiveness of insulin in the body and brain. Insulin is mainly produced by the pancreas. The pancreas is not the only organ to produce insulin, neurons within the brain produce also insulin. Insulin is essential for neuronal function, especially memory and cognition.
Reducing the effectiveness of insulin within the body can contribute to some of the physical hallmarks of Alzheimer’s Disease in conjunction with memory loss and decreased cognition. In one review article, insulin resistance from Type II Diabetes Mellitus completely disrupts normal neuronal functioning. Typically, insulin and insulin growth factors stimulate insulin receptors, which activates IRS, recruiting PI3K, which activates Akt. Akt will deactivate GSK3b, and Akt will go on to activate transcription factors, such as mTor. mTor will activate genes in the neuron to produce more insulin receptors, as well as helps the neurons to grow and survive, as seen in Figure 2.
When insulin receptors are no longer stimulated to the same capacity by insulin and insulin growth factors due to insulin resistance, IRS, PI3K, and Akt activation is decreased or completely stopped, which will allow GSK3b to become overactive. This protein can decrease a neuron’s capacity for growth and life by producing factors within the neuron that stimulate death, as well as neurofibrillary tangles (NFT) and amyloid beta (Ab) plaques, seen in Figure 2. NFT and Ab plaques are hallmarks of Alzheimer’s Disease. These buildups are toxic to neurons and cause neuronal death, which is why symptoms of impaired cognition and memory loss are common in Alzheimer’s Disease.
 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6255119/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6255119/
NFT and Ab plaques can be regulated by insulin. Insulin can help to clear Ab plaques and helps to stop NFT formation, which is why insulin resistance is being looked at for potential therapies to treat Alzheimer’s Disease. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6255119/
Now what?
Alzheimer’s Disease does not have a cure, but exciting research is being done on drugs that target the insulin pathway to slow and potentially stop the progression of Alzheimer’s. One major factor that can be controlled is diet and exercise. By reducing the amount of saturated fat and sugar in the diet can decrease the likelihood of developing insulin resistance later on in life. Exercise can decrease precursors of saturated fat in the blood and muscles, which promote insulin resistance. https://www.frontiersin.org/articles/10.3389/fendo.2019.00577/full
Why care about Alzheimer’s?
Alzheimer’s Disease not only takes a toll on people who are diagnosed with this disease, but also their families. More and more people are becoming diagnosed with this, especially in the United States, and more preventative care and treatment options need to be developed.
Forgetting to Live Healthy
Introducing the problem
As advanced as modern medicine is, there are still anomalies which have the scientific community confused. Increasingly Alzheimer’s disease is gaining attention as it becomes more prevalent in society. While chronic diseases take a toll on the patient, there are few more devastating than Alzheimer’s. Friends and family have to sit on the sideline and watch as loved ones deteriorate into an unrecognizable shell of their former self. While we wait for a pharmacologic silver bullet, there are ways to buy time. By simply understanding the basics of the disease we can make lifestyle changes to swing the odds in our favor.
Getting to the root of the problem
To understand Alzheimer’s, you must understand Amyloid plaques and Neurofibrillary tangles (NFTs). These are the two physiologic trademarks of Alzheimer’s. They stimulate changes in the brain like neuroinflammation and neural cell death. The question we ask then is about the origin of these dysfunctions in the brain. Research is pointing in the same direction as the well-known disease Diabetes.
Insulin is a hormone in the blood which helps regulate blood sugar levels by breaking down glucose and redistributing it as energy throughout the body. Insulin resistance occurs when there is consistently too much sugar in the blood stream and the body’s cells begin to react differently to the hormone. In the body this is the hallmark cause of type 2 diabetes, in the brain it may be the leading cause of Alzheimer’s.
Insulin resistance and its affects
In the brain, insulin resistance affects different signaling pathways which normally have healthy regulation and affects. When insulin receptors are bonded PI3K is activated, this leads to the activation of the protein kinase AKT which inhibits GSK-3B. Conversely, PI3K disruption is responsible for the hyperphosphorylation of TAU proteins, which are the main component of NFTs. Also, when GSK is not activated it leads to the deposition of Amyloid plaques. This is not the only pathway affected by insulin resistance. The MTOR pathway is activated by PI3K and its normal function is healthy, when disrupted it leads to TAU phosphorylation and AD pathogenesis. “Insulin resistance boosts the detrimental forces like oxidative stress, cytokines production, and apoptotic process. These phenomena instigate the neurodegenerative process causing impairment in memory and cognitive behavior”-https://moodle.cord.edu/pluginfile.php/1052906/mod_resource/content/1/insulin%20signaling%20and%20AD%202020.pdf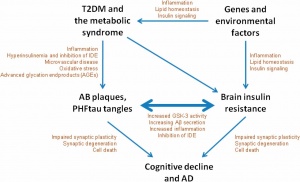
While we cannot directly control the signaling pathways in our brain, we can control our blood sugar levels by eating healthier and being more active. There are also other external risk factors we can limit to help reduce the odds of developing AD. Oxidative stress caused by fatty diets can cause neuroinflammation. There are also correlational studies linking stressful lifestyles, specifically occupations, to increased chances of developing AD. The most important external factor we cannot control. Age is the biggest risk as we see the eventual death of brain cells with aging.
Conclusion
While there is no magic pill a person can take to cure Alzheimer’s there are things a person can do to help limit your chances of developing this terrible disease. Being mindful about diet, exercise, and personal stress levels can increase your chances of growing old without losing your memory.
Hmmmm…. APOE…. why should I care?
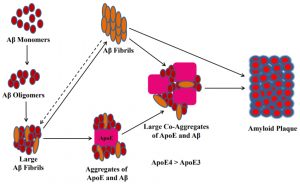
 We’ve spoken quite a bit about the impacts that amyloid plaque can have on the anatomy of our brains, and subsequently how those changes in anatomy can have negative effects on our cognitive function. But in case you forgot I will provide a brief overview. Plaques accumulate over time naturally, however, in Alzheimer’s our brain fails to keep up with the demand for clearance and is therefore overwhelmed by the buildup of these plaques. The abnormal levels of these plaques clump together and are found positioned between neurons, ultimately disrupting cellular function as shown below (U.S. Department of Health and Human Services).
We’ve spoken quite a bit about the impacts that amyloid plaque can have on the anatomy of our brains, and subsequently how those changes in anatomy can have negative effects on our cognitive function. But in case you forgot I will provide a brief overview. Plaques accumulate over time naturally, however, in Alzheimer’s our brain fails to keep up with the demand for clearance and is therefore overwhelmed by the buildup of these plaques. The abnormal levels of these plaques clump together and are found positioned between neurons, ultimately disrupting cellular function as shown below (U.S. Department of Health and Human Services).
Consider for a moment that we could simply remove these plaques, it may not solve our problem entirely but perhaps it could lead to a decrease in negative symptoms momentarily. Lucky for us the advancement of technology has provided new techniques to not only decrease amyloid plaque formation initially, but to potentially remove it from an area entirely after is has begun to accumulate.
It might be helpful to first provide some background information that is required to understand the topic. Embedded within an amyloid plaque lies a protein called APOE. APOE is located near the center of the amyloid-APOE complex and is accessible from the exterior given the right circumstances. These complexes come together with AB Fibrils, proteins that are initially soluble but become insoluble after their assembly is altered, this combination is what forms the amyloid plaques that we are so used to talking about. You can see this without my poor explanation in the figure shown below.
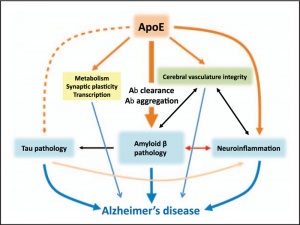
Changes in APOE proteins are thought to be one of the largest risk factors for Alzheimer’s, different unnatural changes to the protein can lead to differing severities of the disease. The figure below demonstrates the negative side effects that can come from the unnatural variations of APOE.
Researchers at Washington University recently discovered antibodies that can target and initiate removal of plaques from the brain by directly binding to the APOE domains. By doing this the antibodies effectively flag the compound for degradation by the local immune system. Although it is meant to be a humorous take on the immune systems response to APOE, the picture that I altered may help you remember this point.
When these immune cells target the APOE, scientists discovered that the immune cells would also carry away the connected amyloid plaque that had formed around the APOE. In this situation you can think of the APOE-plaque complex as the metaphorical saying “throwing the baby out with the bathwater,” except in this case it’s a positive.

It should be noted however, that there is a caveat to this claim relating to the removal of plaques via antibody binding. Scientists believe that using antibodies may only be effective during the early stages of amyloid plaque build-up. The scientists from Washington noted that if too much plaque is present, that the addition of antibodies might not be enough to counteract the inevitable disease that is Alzheimer’s.
“Okay,” you might say, “but surely APOE has other important roles in the body, degrading all of it would be bad.” And indeed you would be right, APOE does have other important roles in the body such as “the transfer of cholesterol and phospholipid between cells” (Liao et al, 2017). Luckily however, researchers found an antibody that only affects the APOE in the brain and not throughout the rest of the body. Initially the researchers were stumped as to why the antibody (antibody HAE-4) only affected the APOE in the brain. But of course, someone else had done their research for them, it turns out that there are three different naturally occurring isoforms of APOE. Different isoforms are present depending on the region of the body, the brain having its own individual isoform entirely (from what I gathered from the article). This difference allows antibodies, and therefore researchers, to target the brain’s APOE without worrying about damaging the subject. Because of this discrepancy, researchers can potentially use antibody technology to prevent Alzheimer’s disease in the future.
Sources
Liao, F., Yoon, H., & Kim, J. (2017, February). Apolipoprotein E metabolism and functions in brain and its role in Alzheimer’s disease. Current opinion in lipidology. Retrieved September 27, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5213812/.
ScienceDaily. (2018, March 26). Antibody removes alzheimer’s plaques, in mice. ScienceDaily. Retrieved September 27, 2021, from https://www.sciencedaily.com/releases/2018/03/180326161000.htm.
U.S. Department of Health and Human Services. (n.d.). What happens to the brain in alzheimer’s disease? National Institute on Aging. Retrieved September 27, 2021, from https://www.nia.nih.gov/health/what-happens-brain-alzheimers-disease.
Road Block on Mental Health
Stigmatization and Schizophrenia
Schizophrenia, as well as other psychotic and mental illnesses, are often the targets of stigmatization. It is unfortunately very common for those with Schizophrenia, or many other invisible illnesses for that matter, to face some form of stigmatization. Stigmatization, known as a group of stereotypes correlated with false beliefs, negative attitudes, and fears about a Schizophrenia diagnosis which results in the perception and comprehension of the disorder by others https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659317/. Stigmatization, which is often characterized as an external risk factor that can project its characteristics in many ways, may impact someone after they are given a diagnosis, but also can happen prior to a diagnosis, through small and subtle behavioral expressions of Schizophrenia https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659317/. An example may be judging someone due to speech differences or behavior that is stereotypically linked to Schizophrenia.
For Every Action, there is an Equal and Opposite Reaction
For one struggling with Schizophrenia, these harsh and false beliefs from others is hypothesized to cause negative psychological outcomes in the mentally ill, including those with Schizophrenia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659317/ Those with mental illness are already often socially rejected, which has a great impact on one’s general well-being and self-esteem. Someone may feel more depressed, anxious, isolated, embarrassed, scared, or angry. It is not unlikely for those with Schizophrenia to also have a social anxiety related disorder, so this added stigma only perpetuates the already isolating and adverse journey of Schizophrenia. Also, stigma only stops others from getting the help that they need.
What can be done?
Like most of us were instilled growing up, “Treat others how you would want to be treated.” How we view and treat others always comes with consequences. The choice is ours.
- W.A.I.T.: “Why am I talking?”
- Over the summer, I read a book that shared the acronym, “W.A.I.T.,” which stands for “why am I talking?” Since learning of this acronym, I have more often found myself thinking through my thoughts before blurting meaningless word jumble. Basically, think before you respond. Is what you are about to say helpful or harmful? To yourself? To others? When it comes to communicating about mental illness, ask yourself to WAIT. Figure One shows how judgement, stigma, and mental illness are all connected and how practicing “W.A.I.T.” can stop the cycle.
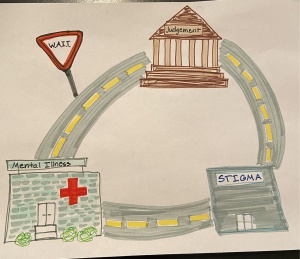
Figure 1: This abstract shows the stigma cycle that is often associated with mental illness and how simple techniques like “WAIT” can stop the cycle.
- Recognition Between Mental and Physical Illness
- You would not make fun of someone with cancer, a broken leg, or a physical disability. When you can recognize and understand that mental illness, like physical illness, is a disease, you may find yourself become hesitant to judge someone.
- Educate Yourself
- Before judging someone else, educate yourself. Ask someone else to share their story or personal experience, you may be surprised and humbled to learn about someone else’s journey. Always try to find the learning opportunities to help you grow in understanding and compassion for others struggles. Deepening your understanding and awareness disrupts the cycle of stigma.
- Choose Compassion
- Recognize the humanity of mental illness; the vital fact that every single human is vulnerable. We are all more alike than we are different. Choosing to show compassion through a simple, “hello” to a fellow human unifies us and reminds the world of what can happen when we choose compassion over judgement.
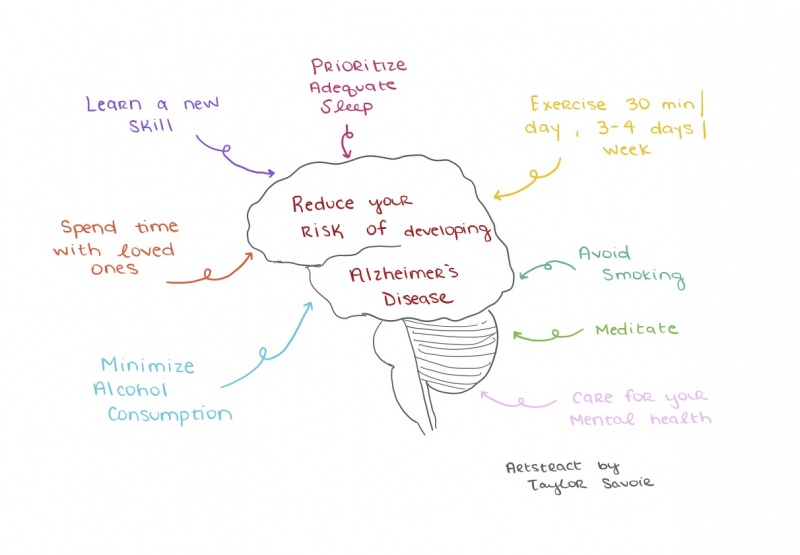
8 Ways to Decrease Your Risk of Developing AD
Insulin Signaling Pathway’s Relation to Alzheimer’s Disease
Alzheimer’s disease is identified by a buildup of amyloid-β plaque and neurofibrillary tangles (NFTs). Insulin signaling is disrupted in patients with AD leading to the increase of plaque and NFTs. Molecules such as Akt, mTOR, Grb, and RAS have decreased activation in patients with AD. Other molecules are overactivated because of insulin dysfunctions like SOS, MAPK, and GSK-3β. Figure 1 is a simple flow chart I drew of the molecules in the insulin signaling pathway; the green or red arrow next to the molecule signified whether it has increased or decreased activation in patients with AD.
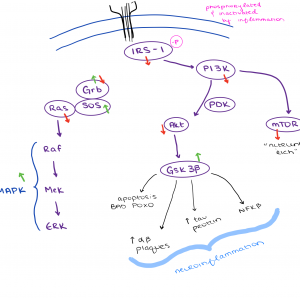
Figure 1: The insulin signaling pathway is dysfunctional in patients with AD.
When these molecules are under or over-activated, insulin abnormalities can lead to insulin resistance. Insulin resistance is linked with the build-up of amyloid-β plaque and NFTs. Patients diagnosed with Type 2 diabetes have increased chances of developing AD because both of these diseases are characterized by insulin signaling abnormalities and insulin deficiency.
Why should we care?
The public should care about Alzheimer’s Disease (AD) because developing it can be greatly impacted by someone’s lifestyle choices. There is no cure for this disease, but increased research of causational factors, early symptoms, and education about it will decrease the number of cases in the future.
Humans have adapted harmful lifestyles that are expected to offset any decreases seen in the AD cases. Especially in the United States, many people smoke, have high body mass indices, and consume large amounts of sugar, fat, and cholesterol. The amount of people with AD has been increasing for decades and is projected to continue growing. Humans live longer than ever before and that is not without its difficulties. The following video from the Alzheimer’s Associated provides a summary of the facts and figures of AD and their projected numbers in the future: https://www.alz.org/alzheimers-dementia/facts-figures/
8 Ways to Decrease Your Risk of Developing AD
There is not one thing in particular that causes Alzheimer’s Disease, but we know about many life choices that can alter your chances of developing it. While living with AD is not on most people’s minds throughout the day, the ways in which we spend our time can help reduce the risks of developing symptoms. The most effective way to prevent Alzheimer’s is to start making the following choices early, consistently, and effectively.
- Learn a New Skill – The brain will form new synaptic connections when exposed to new stimuli. It is beneficial to consistently learn something new in order to decrease your risk of developing AD https://alz.org/aaic/releases_2021/global-prevalence.asp.
- Spend Time with Loved Ones – Strong social interactions are linked to stronger neuron connections and preventing neurodegeneration. Experts are not exactly sure how social stimulation does this, but there is evidence to support the hypothesis.
- Minimize Alcohol Consumption – Excessive use of alcohol can damage brain cells over a period of time. Decreasing the amount of alcohol one drinks can decrease the likelihood of developing AD.
- Prioritize Adequate Sleep – People who get more hours of deep sleep (REM cycle sleep) are less likely to develop AD. Researchers hypothesize that this is because the brain clears out waste during REM sleep that has been linked to AD. https://www.npr.org/sections/health-shots/2020/11/17/935519117/deep-sleep-protects-against-alzheimers-growing-evidence-shows
- Exercise – Experts recommend getting vigorous exercise for 30 minutes a day, 3-4 days a week to experience maximum health benefits. Exercise reduces the risk of cardiovascular disease, diabetes, and neurodegenerative diseases, which can be closely linked to each other. https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/expert-answers/alzheimers-disease/faq-20057881
- Avoid Smoking – Smoking can cause oxidative stress, inflammation, and cancer. It provides no benefits to the human body and only does harm. Avoiding smoking can decrease the risk of developing AD, cardiovascular disease, and brain hemorrhages. https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/expert-answers/alzheimers-disease/faq-20057881
- Meditation – Meditation has been practiced for centuries, but researchers must conduct more experiments to learn about the specific benefits it can provide. People who practice meditation report lower levels of stress than those who do not meditate. High-stress levels are positively correlated with the chances of developing AD; meditation can reduce stress which, therefore, can reduce the chances of AD.
- Care for Your Mental Health – Mental health is strongly linked to physical health. It is important to minimize stress levels, maximize time spent doing things you enjoy, and prioritize caring for yourself. A healthy body needs a healthy mind to take care of it https://alz.org/aaic/releases_2021/global-prevalence.asp.