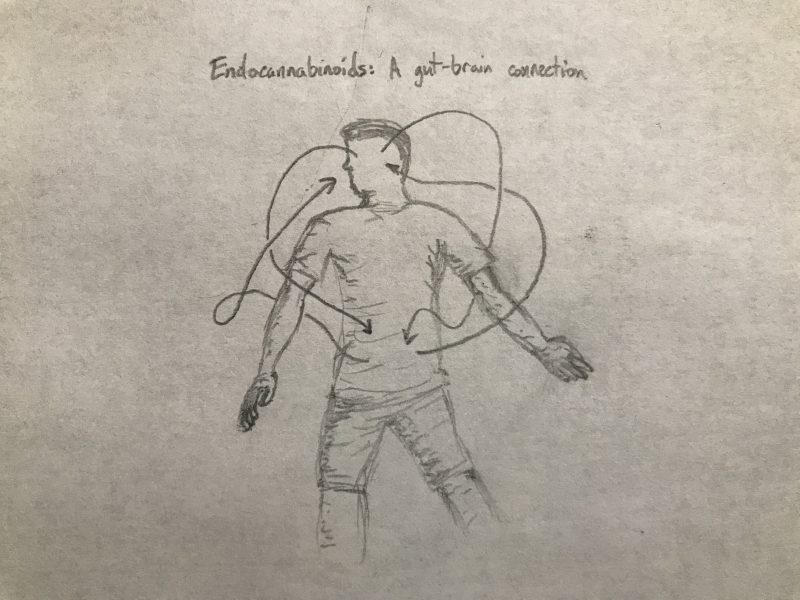
Your brain controls everything in your body right? Well, somewhat. In the case of some reflexes, the signal to pull your hand back from something hot may not have actually traveled to your brain until you’ve already completed the motion. On another level, there is evidence that the gut may also function somewhat independently, and actually communicate much more with the brain than previously thought. In some ways we already know this is true. When you’re standing in line for a roller coaster, you might feel a little nervous, and your stomach starts to turn. This is your brain and gut communicating, and this talk is a two way street. Both affect each other heavily, which can be positive or negative, depending on the situation.
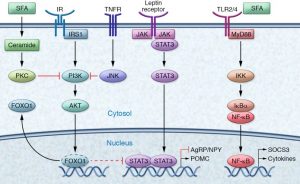
If the gut microbiome is disturbed (reasons can include stress, low fiber, sleep  disturbances, etc.), this appears to not be great for our overall health. These disturbances typically lead to a low grade, local inflammation of the gut, which then turns systemic. Because of the gut-brain connection, systemic inflammation becomes neuroinflammation, or inflammation of the brain’s tissue. This can have all kinds of adverse effects that can show themselves behaviorally, or change the way the brain functions. Since the gut can affect the brain negatively like this, there are also positives that can occur. One of the major upsides that research is looking into is that we may be able to address and treat issues that are commonly associated with the brain, such as anxiety and depression, through the gut.
disturbances, etc.), this appears to not be great for our overall health. These disturbances typically lead to a low grade, local inflammation of the gut, which then turns systemic. Because of the gut-brain connection, systemic inflammation becomes neuroinflammation, or inflammation of the brain’s tissue. This can have all kinds of adverse effects that can show themselves behaviorally, or change the way the brain functions. Since the gut can affect the brain negatively like this, there are also positives that can occur. One of the major upsides that research is looking into is that we may be able to address and treat issues that are commonly associated with the brain, such as anxiety and depression, through the gut.
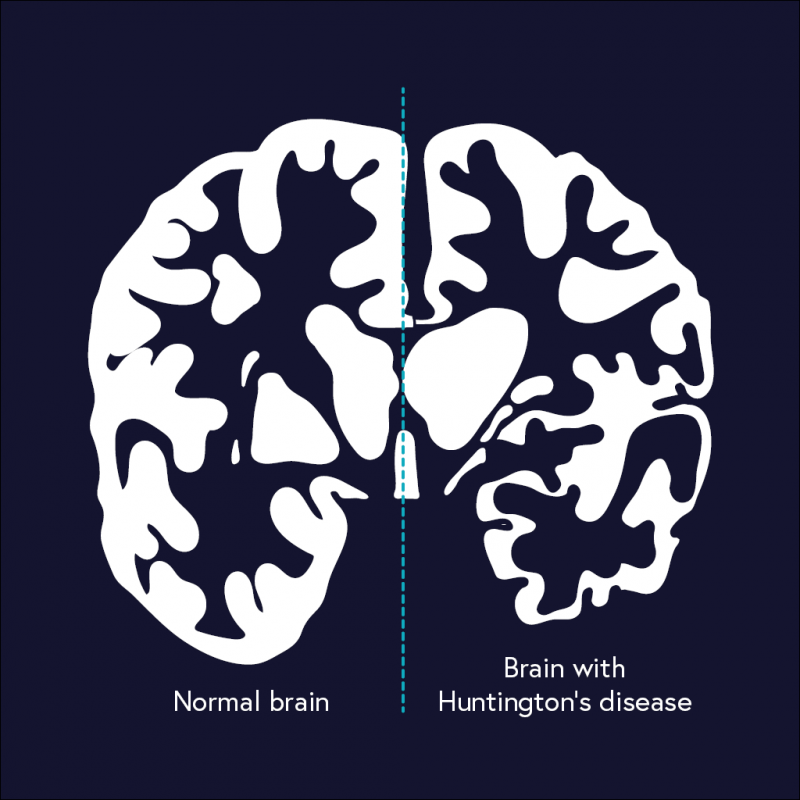
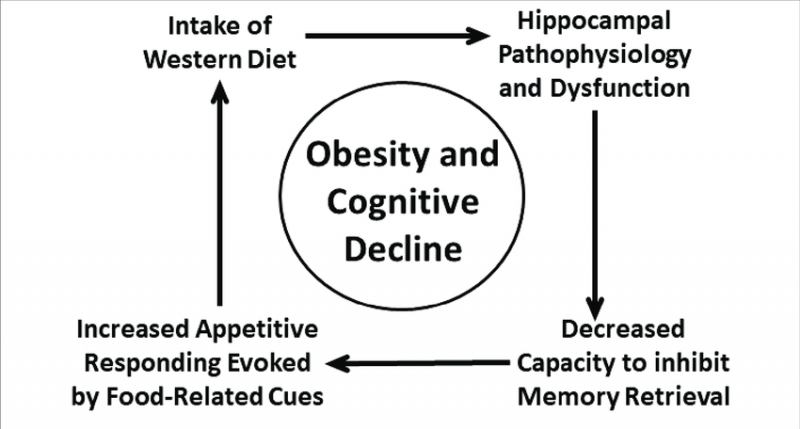
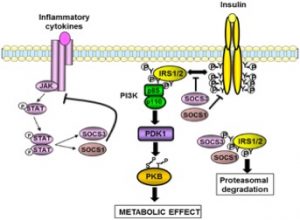
When the gut is inflamed, it has been found that endocannabinoid signalling is lower than it should be (and yes, endocannabinoids relate to cannabis). It makes sense then that restoring proper levels of endocannabinoids would help to treat inflammation. Using neuroinflammation as an example, restoring this endocannabinoid signalling to the gut relieves neuroinflammation as well, helping to make the entire body work more smoothly. As talked about in my obesity blog post (shameless plug), inflammation can perpetuate and worsen obesity, which can increase insulin resistance, which, as talked about in my Alzheimer’s post, can lead to neurodegenerative diseases such as Alzheimer’s disease or Parkinson’s. Basically, inflammation is really not great, and can cause a cascade of negative effects that can happen over a period of decades. The good news though, is that inflammation can be treated using endocannabinoids, but that also doesn’t mean we shouldn’t try to prevent inflammation in the first place.
to neurodegenerative diseases such as Alzheimer’s disease or Parkinson’s. Basically, inflammation is really not great, and can cause a cascade of negative effects that can happen over a period of decades. The good news though, is that inflammation can be treated using endocannabinoids, but that also doesn’t mean we shouldn’t try to prevent inflammation in the first place.
Something interesting that has been found in this gut-brain link is the ability for the gut to moderate pain and how we perceive it. Chronic pain that doesn’t have a reason to be painful (as in there isn’t any reason for pain to occur), also called neuropathic pain, is a common thing among Americans. Endocannabinoids moderate this pain, and so if someone is struggling with chronic pain of this sort, increasing their endocannabinoid levels can help alleviate pain (along with inflammation that can go along with the pain!).
With all this being said, it’s important to do what your grandma probably told you, eat well, do things you like to do, and sleep well and often, and your endocannabinoid levels and gut will thank you for it. Ok, she might not have said that last part, but I bet she was thinking it.

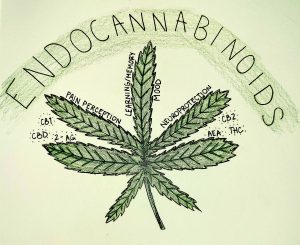
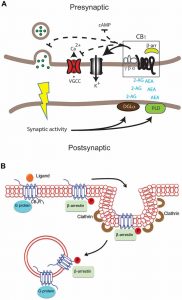

 Because the endocannabinoid system assists with memory, reduction of inflammation, and protection from neurodegeneration, it makes sense that dysregulation of the system could play a role in Alzheimer’s Disease. Evidence also supports a role of the system: levels of key molecules are off in AD brains and CB1 and CB2 receptors are correlated with tau tangles and other hallmarks of AD.
Because the endocannabinoid system assists with memory, reduction of inflammation, and protection from neurodegeneration, it makes sense that dysregulation of the system could play a role in Alzheimer’s Disease. Evidence also supports a role of the system: levels of key molecules are off in AD brains and CB1 and CB2 receptors are correlated with tau tangles and other hallmarks of AD.