Are You Addicted?
Everyone, take a moment to pull out your cellphone, go into your settings, and look at your daily average screen time. I’ll give you a moment as you pass through the five stages of grief. You are probably currently trying to justify the absurd amount of time you spend on the device. Think back to when you’ve missed placed your phone and the slight sense of panic that followed as you desperately searched for your device. We keep the little device on us at all times and everywhere you go you can find someone looking at the mesmerizing screen. We can’t seem to separate ourselves from these pieces of technology, depending on them to store information and remind us about it later, show us the way when going anywhere, solving problems, and run calculations for us and entertaining us. How many of you look at your phone while using the restroom? That’s what I thought, you may be addicted to your phone. Addiction can present itself in numerous ways such as drug, sex, food, caffeine, and technology addiction along with many other forms.

What Is Addiction?
So, what is addiction anyway? Addiction is experiencing a strong sometimes irresistible repeating impulse to pursue some behavior that triggers the reward pathway within an individual and creates a need or dependency for that reward sensation through repetition of the behavior. Addiction can be associated with sensitization, compulsive behaviors, loss of control, dependency, withdrawal, tolerance, and even relapse. One of the most common and well-recognized forms of addiction is drug addiction. Drug addiction can be very destructive and is a serious condition that shouldn’t be taken lightly alongside the many other forms of addiction.

How Does It Happen
In the case of drug addiction, the addiction aspect arises from repeated use of the substance which generates a positive sensation. This repetition in use promotes physical changes to the individual’s brain making them more susceptible and more likely to continue seeking the substance. If this individual continues to use the substance, they may eventually lose control over the use of the drug creating a further perpetuating cycle of dependence. Because of the physical changes within the brain, addiction can be extremely difficult to overcome and can have serious long-lasting effects. As an individual uses a substance, they begin to alter the brain’s sensitization to the drug meaning the neurons change their shape and connectivity to either increase or decrease their engagement with the substance. The brain adapts by developing a tolerance to the drug which neutralizes its effects requiring the individual to continually consume larger and larger quantities of the substance to experience the same stimulation they had the first time they used it.
Once addicted the individual experiences a need and severe craving for the substance due to the physical changes within the brain. If the user attempts to stop using the drug they experience severe negative symptoms including withdrawal that make it incredibly difficult to stop using the substance.

Why Does It Happen?
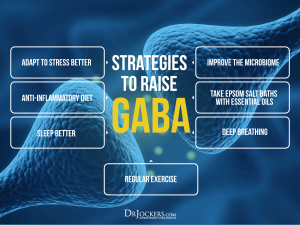
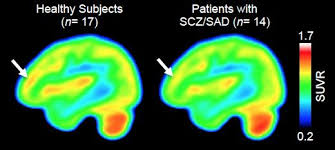
In drug addiction, the drugs bind to specific receptors in the brain typically within the Ventral Tegmental Area (VTA), and stimulate neural cells that interact with the Nucleus Accumbens (NAc) which is a reward pathway within the brain. This activates a cascade of signaling within the neural cells which ultimately leads to the activation of important transcription factors abbreviated as CREB and delta-FosB, along with many others that regulate the transcription/production of genes within the cells. The neural cells function based on the genes that are transcribed and their quantities. These changes in gene transcription result in the cells changing shape and increasing or decreasing receptors on their membranes (makes it easier or harder for them to interact with the drug), which ultimately affects the desires and behaviors of the user.
Sources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3898681/
https://www.psychiatry.org/patients-families/addiction/what-is-addiction
https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction



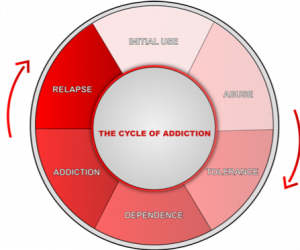 rough various “stages” as they continue to abuse the substance or behavior to which they have become addicted. The cycle also helps explain why most people don’t have a few drinks at a social event and wake up the next day as an alcoholic—addiction is a long, strenuous process where several circumstances have to line up in order for that person to become addicted. The cycle can be extremely challenging to escape, which accounts for the disheartened attitude seen so often in addicts seeking treatment. While the cycle may be seen as unescapable, even the most severe cases of addiction are treatable. Getting professional help is the way out and the way to a higher quality of life unaffected by the addictive substance or behavior.
rough various “stages” as they continue to abuse the substance or behavior to which they have become addicted. The cycle also helps explain why most people don’t have a few drinks at a social event and wake up the next day as an alcoholic—addiction is a long, strenuous process where several circumstances have to line up in order for that person to become addicted. The cycle can be extremely challenging to escape, which accounts for the disheartened attitude seen so often in addicts seeking treatment. While the cycle may be seen as unescapable, even the most severe cases of addiction are treatable. Getting professional help is the way out and the way to a higher quality of life unaffected by the addictive substance or behavior.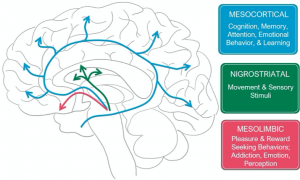 The mesolimbic pathway (pink/red in the
The mesolimbic pathway (pink/red in the 




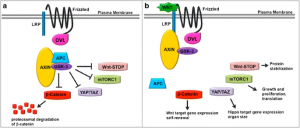
 Imagine if a skyscraper were constructed in such a way where they needed constant maintenance, and if they did not get it would be there natural state to collapse and be destroyed. It seems like a real backwards way to construct a building, or to maintain anything man-made or natural for that matter. So it is surprising to find out that a major chemical signaling pathway, the Wnt and GSK pathway, operates in manner that aligns with this metaphor. The natural state of this critical signaling pathway is that of destruction. The pathway must be activated by a Wnt ligand that triggers cellular events that stop a complex that is involved with destruction. If that seems a bit confusing, I was with you but bear with me. The pathway must be activated, to stop intracellular destruction, which maintains normal cell development.
Imagine if a skyscraper were constructed in such a way where they needed constant maintenance, and if they did not get it would be there natural state to collapse and be destroyed. It seems like a real backwards way to construct a building, or to maintain anything man-made or natural for that matter. So it is surprising to find out that a major chemical signaling pathway, the Wnt and GSK pathway, operates in manner that aligns with this metaphor. The natural state of this critical signaling pathway is that of destruction. The pathway must be activated by a Wnt ligand that triggers cellular events that stop a complex that is involved with destruction. If that seems a bit confusing, I was with you but bear with me. The pathway must be activated, to stop intracellular destruction, which maintains normal cell development.