The Neurochemistry students are back, writing about all sorts of interesting data and social issues that come with the discussion of the brain!
Enjoy reading….

The Neurochemistry students are back, writing about all sorts of interesting data and social issues that come with the discussion of the brain!
Enjoy reading….
I cannot thank Concordia enough for the opportunities it has provided me during my four years of enrollment. Not everybody has the privilege of obtaining a liberal arts degree that promotes interdependence and exploration of other fields. While other courses have been a major influence in my growth and development in college, neurochemistry has given me a chance to implement all that I have learned thus far. As my capstone experience, the class was structured to give students an opportunity to become responsibly engaged in the world (BREW) while still receiving support from Concordia’s faculty and services.
The class required the planning, implementation, and analysis of a community action project focused on Autism in our society. We first had to figure out the needs of our community and what type of project could aid in the public’s knowledge, understanding, and acceptance of the disorder. In a group of nine students, we researched and collaborated what options would be most beneficial to the Fargo Moorhead area. We finally decided to hold an interactive workshop for the education majors at Concordia College since they will become the next generation educators who interact with autistic students on a daily basis. After reaching out to many experts, we focused our project content on three simple aspects that can be overlooked by teachers in their classrooms. The first main point we discussed was how to appropriately start a parent-teacher relationship without being condescending or accusing. The next was to emphasize the importance of early intervention and screening for all children because it only can benefit the development of our students and future children. Lastly, we made sure to incorporate some teaching strategies and techniques that are beneficial for all students, but extremely crucial for those with autism.
Our project went exceptionally well and we had great feedback from those who attended. However, the project did not come without a lot of hard work, intensive communication, especially between our nine-membered group, and many challenges. The entire project was aimed towards education majors at Concordia and we only had 3 or 4 show up to our event with the majority being students from other majors. Again I think this information is really beneficial to anyone but extremely necessary for those going into teaching jobs in the near future. Another challenge we faced was contacting people outside of Concordia to possibly talk at our event. It was a major learning experience to understand how hard it is to organize events and coordinate public functions. Even if you have the most valuable information in the world, if you can’t organize efficiently, advertise thoroughly, and effectively present your information, then none of it matters.
It was also beneficial for us to work with another discipline, like social work, to complete this project. It taught us how to be professional but assertive during group meetings and also expanded our field of view about the topic. The neuroscience majors were able to bring in the science behind Autism while the social work students were able to talk about family life, school system, and other aspects of the disorder to give our audience a holistic understanding of the disorder. Also as future doctors, dentists, and scientists, this was a crucial opportunity for us to practice talking to the general public about complicated issues. In our near futures, we are going to be expected to explain diagnosis, procedures, treatments, and medicine to any individual. Another valuable outcome of this project was the realization of my own personal biases and perceptions I had about Autism. Before talking to people personally affected by Autism, I had no idea how much of a financial and emotional toll it has on a family. Lastly, this class as a whole has fueled my love for lifelong learning. Without as many assignments or deadlines, it gave us the freedom to explore the topics as we pleased. Some people would take advantage of this freedom and put in minimal effort, but I feel like our class did a great job of wanting to deep deeper and learn more for our own personal benefit. It was such a fun atmosphere that not only pushed me as a student but as an active member of my community.
Out of all the science courses I have taken at Concordia College, Neurochemistry was the only one that truly encapsulated the meaning of BREW, or Becoming Responsibly Engaged in the World. In this class, we were meant to make a difference in the community in some fashion, pertaining to a neurodegenerative disease or disorder. I am fairly confident we all were able to accomplish this. In my case, my group and I were able to educate others on autism and some guides on how to effectively teach a child with autism in the classroom. In our group, we had several people, many of whom had varying degrees of experience with autism. Some had grown up with friends that had autism, worked with autistic children at their job, or even had a family member with autism. Together with our different specialties in school, we had a diverse perspective on the disorder and the information we would like to share. We were never going to be able to give a comprehensive “how-to” that works for every child, but I believe the tips from us and our guest expert, Cailin, could be a useful aid. Even though the message wasn’t as widespread as we would have liked, the few educators we were able to connect with highly valued the information.

Coming into this course, I knew very little about the brain, especially when it comes to all the neurological disorders we discussed (except for maybe concussions). I didn’t anticipate to, but I enjoyed reading the scientific papers; they just added so much to my knowledge base on these real world problems we come in contact with or discuss on a regular basis. Even more so, once we were able to dig to the root of these papers, much of it just made sense, and you could see connections to other courses (for me, namely biochemistry and genetics). They also were able to change some of the common misconceptions or stigmas I had on some diseases (especially when it came to addiction and schizophrenia).
There is also something to be said for the value we gained in constantly speaking in scientific terms, and then transferring it into more simpler terms when we get the chance to discuss what we’ve learned to others. It’s helpful not only for being able to inform others on the awesome research that’s being done today, but even help ourselves with understanding it more thoroughly.
I’m unbelievably grateful for having the opportunity to take this course; I think every person should learn the information we did in this class. Neurochemistry really did culminate into a top academic experience where the students could grow in our skills as communicators, researchers, and difference-makers. I anticipate the things I have learned here to translate into my future graduate research (or research goals at least!).
3.5 years of struggling at this point with many hours of studying, pain, tears, joy, hope, dedication, and perseverance. At points the entire college thing completely sucked, and sometime still sucks, *cough* *cough* finals. One specific example that comes to mind is receiving a truly failing grade on an exam in a required course and yet leaving the course with a B and testing within the top 10% of the nation.  The years were hard and at times but I would not trade it for the world. I have made many friends, learned astronomical amounts of information that sometimes felt insignificant, paved the way for the future students, became responsibly engaged in my community, and ultimately grew as a person. I am proud to be where I am today because of Concordia, and this class did a great job of highlighting that. So I say thank you Concordia, thank you to all the faculty who have taught me not only textbook materials but life skills. Thank you to all the people that supported me, to all the friends I have made and to those who have been essential in shaping who I am today. Thank you for your liberal learning practices and allowing me to grow, not only as a student but within the world, for my critical thinking and reasoning skills, and for making me a better and more informed person. There is nothing left to say but thank you. As of now, the light at the end of the tunnel is visible and though I do not know what is on the other side, I walk to it gladly, awaiting the new adventures to be found. When I walk across that stage this May I will be forever proud to call Concordia my alma mater.
The years were hard and at times but I would not trade it for the world. I have made many friends, learned astronomical amounts of information that sometimes felt insignificant, paved the way for the future students, became responsibly engaged in my community, and ultimately grew as a person. I am proud to be where I am today because of Concordia, and this class did a great job of highlighting that. So I say thank you Concordia, thank you to all the faculty who have taught me not only textbook materials but life skills. Thank you to all the people that supported me, to all the friends I have made and to those who have been essential in shaping who I am today. Thank you for your liberal learning practices and allowing me to grow, not only as a student but within the world, for my critical thinking and reasoning skills, and for making me a better and more informed person. There is nothing left to say but thank you. As of now, the light at the end of the tunnel is visible and though I do not know what is on the other side, I walk to it gladly, awaiting the new adventures to be found. When I walk across that stage this May I will be forever proud to call Concordia my alma mater.
Neurochemistry was a capstone course, my capstone course. It was the course that was to be part of the final over-encompassing conclusion of my 4 years at Concordia. While I didn’t truly have a choice in my course, due to my specific major, it was a course I would have gladly chosen. I originally heard about Neurochem my junior year from some of the seniors of that year. While it was described as a lot of work, it was also described as one of the most rewarding experiences. I remember the first day of classes, seeing faces I hadn’t seen since before the disciplines split off into their respective fields, Dr. Mach simply walked in casually saying “hey, class” before proceeding to ask us about our summer vacations. There was no rush to get to the material, no rush to go through the syllabus or anything else the first day usually requires. There was simply this relaxed feeling one would get around friends in conversation as we began to get to know each other better. Don’t get me wrong, some of us were still nervous because it was a class and you never truly know what to expect but it allowed us to live in the present moment with each other. I had no idea what to expect of this class but I can say I didn’t expect to get as much out of it as I did. I walked away from this class with new friends and understanding of people that I’ve known (but haven’t truly known) since freshman year, I truly made an impact in my community, and I learned so much about the world around me in a very interdisciplinary lens.
Neurochemistry is simply a course in which we tried to understand neurological problems and how they came to be, this ranged from autism to addiction to schizophrenia to obesity and so many more topics. In my opinion this course qualifies as an ideal capstone course as it truly embodies Concordia’s five goals of liberal learning. So unless you’re a Cobber yourself, you probably don’t understand this capstone idea. Well let me explain it a little and tell you how Neurochem fit into the picture…
According to Concordia’s course catalog (before they switched to PEAK) capstone courses “invite students to apply their liberal learning to significant problems of a global nature.” Ultimately they want us to BREW, or Become Responsibly Engaged in the World.
The 5 Goals of Liberal Learning:
So the community action projects… I like to think of it as the CAP of CAPSTONE. Our project involved going out into the community and working with support professionals to aid in the understanding of anxiety and PTSD. This not only allowed us to become engaged but it truly opened our eyes to the world around us, more specifically the Fargo-Moorhead area in which we have lived for the past 4 years. Going into this project I had no idea some of these support systems were in place let alone this far in the middle of nowhere (it is truly like the middle of nowhere for anyone from the Twin Cities area). I was able to learn how to take my knowledge I’ve accumulated in the past 4 years and present it in a way that benefits everyone, not just fellow scientists. The most rewarding part of this though was not only that we helped a nonprofit in understanding but we indirectly helped the members of the community (their clients) as certain ideas we presented were actually implemented into their programs and are working to help improve the lives of their clients through managing and reducing their anxiety.
I can not say anymore how great this course was or how much I grew within it. The only thing I will say, again, is thank you. Thank you Concordia and thank you Dr. Mach for giving me this experience. 
– Samantha Beckman; Class of 2019
Image Source: https://image.tmdb.org/t/p/w1280/ApuCppLxFVm8B1NRecs0L8ej4Tj.jpg meme: by me
As a Cobber going into their senior year, needing their peak course, there were a lot of options of classes that I had to choose from. I had heard of the dreaded horrors of microbio, other classmates constantly complaining about embryology, and other laments about other capstone or PEAK classes. Then I heard from Brooke Maruska how great this class called neurochemistry was. And somehow, through the Grace of Concordia College, one of the best teachers on the planet also teaches it. All of those factors caused me to sign up for this class, even though I absolutely VOWED to never take another Chemistry class here again.
I stepped into syllabus day with a huge smile on my face as Dr. Mach strolled through the door and greeted us with her patented, “Hey, class”, and suddenly, I knew, that I had made the right choice. Some faces around me were familiar, others not so much, but by the end of the year, we came together through class-wide chats, where I can say I genuinely made new friends.
Through this year, we spent hours discussing every day pathology of diseases that we see that are prevalent around us, Alzheimer’s, autism, schizophrenia, CTE, and bipolar disorder, just to name a few. And through this class, we learned things about ourselves and the world that I will carry with me for the rest of my life. This class is the ideal Concordia capstone course.
A capstone is a class that carries 5 main values;
Instill a love for learning: Dr. Mach is literally one of the best teachers at Concordia in the fact that she makes you care about what you’re learning. This is the second class I’ve had the opportunity to take from her (Biochemistry being the first) and I can say that she has made learning so easy to do. These topics that we’ve covered this year will come up in every day life, affecting our loved ones and the ones around us, and it’s super important to understand what is exactly going on behind the scenes of these diseases.
Develop foundational skills and transferable intellectual capacities: Scientific Paper reading is an acquired skill. I like to make the joke that science is a language of itself, and reading scientific papers requires a level of skill that not a lot of people have. After this class, you will be able to read scientific papers with ease, and will be able to find the terms that you don’t understand so you can understand fully the concept of what is going on in the pathology. This is useful for any science class we will have to take in our post graduate schools.
Develop an understanding of disciplinary, interdisciplinary, and intercultural perspective and their connections: This class brings together majors of all sorts, we had neuroscience, biology, psychology, music, and chemistry majors all in one class, intermingling and getting to know each other all year long. The sit down chats and speed dating made a lot of this stuff feel personal, like you’re actually getting to know the person, instead of just the topic they covered that week.
Cultivate an unexamined cultural, ethical, physical, and spiritual self-understanding: This class will absolutely challenge you to think about mental health and other diseases in ways you have never thought of before. Understanding where the issues come from is the number one way to understand the root of the problem.
Encourage responsible participation in the world: BREW BREW BREW BREW. As part of this class, you are required to do a community action project with social work majors. NOW NOW NOW, I understand that sounds like so much work, but let me tell you, it ended up being my favorite part of the year. My group reached out into the community and worked with people with Alzheimer’s, and we tried to implement a personalized type of music therapy in our community, and let me tell you, was that the most rewarding thing seeing that all come together in the end.
I am SO glad I took this class, and I would recommend anyone in the world, regardless of your major, to at least consider Neurochemistry for their PEAK experience.

Just like the average American’s waistband, the prevalence of obesity is growing in America. Dr. Cynthia Ogden, a CDC epidemiologist, published the results of a study of weight in the United States concluding that 31% of adults are obese and 15% of children and teenagers age 6-19 are overweight. The proportion of obese people has been growing steadily for the last few decades.Obesity is a severe problem that every American faces due to the Western lifestyle. Our diets seem to consist of “fast food” cuisine and soda pop to wash down the processed foods. But, in reality, the “fast food” is actually slowing us down. However, you would think that most people would realize that this lifestyle is quite unhealthy. The answer to this question lies inside the brain.
“Severe obesity is not just about eating and activity, it really is a biological condition. It’s the obesity that’s driving the extra eating. It’s the obesity that’s driving limited physical activity, not the other way around.” said Dr. Claudia Fox, a doctor in the Department of Pediatrics at the University of Minnesota Medical.
Obesity can cause insulin and leptin resistance, which under normal conditions balance energy expenditure and food intake. However, under obese conditions, the brain becomes resistant to insulin and leptin, causing one to over-eat. Saturated fatty acids are the molecules of which our fast foods and western diets primarily consist. These molecules can accumulate within the brain, which can lead to inflammatory pathways being activated. This inflammation is what causes insulin and leptin resistance that is characteristic of obesity.
Insulin resistance can then lead to inhibition of POMC neurons. POMC neurons are the set of neurons that tell our brain to stop eating. On the other hand, AgRP neurons are the other set of neurons that become activated under fasting conditions. Once these neurons are activated, they induce feeding, inhibit energy expenditure, and regulate glucose metabolism. Interestingly, POMC neurons become inhibited while AgRP neurons become activated under obese conditions. This leads to a detrimental cycle of eating, and not expending energy.

Fig 1. Correct signaling on the left. Obesity’s effect the signaling pathway on the right. Resistance occurs with obesity, leading to inactivation of POMC neurons and lack of inhibition of AgRP neurons. This promotes increased food intake and body weight gain.
So, what can be done to break this cycle? Dr. James O. Hill, chair of the department of nutrition and food studies at New York University believes that the lack of activity is the culprit behind our growing waist bands. Dr. Marion Nestle, chair of the department of nutrition and food studies
at New York University, agrees, but she lays more stress on eating habits. Both are correct. It is our western lifestyle of instant gratification that has led to us stuffing ourselves with instant, ready-made food. This very food, that is supposed to keep us going, has slowed us down. These two factors, increased food take and decreased energy expenditure, is a recipe for a country “diseased” with obesity. More focus should be placed on eating less and healthier, and also being more active. I know it is easier said than done, but I believe it all starts with awareness. Once more of America becomes aware of what our food is actually doing to their bodies, then, hopefully, they seek help or change their eating and exercising habits.
Neurochemistry is required for the neuroscience major here, as well as a capstone, at Concordia and as I was registering for classes for my final year at Concordia this was the class I felt the most nervous about. I had not taken Biochemistry, a class that I knew would be heavily associated with the class so I knew that I would be behind the rest of the class in regards to that. I qualmed some of my fears about the class by learning that the classmates I would be surrounded with, some of the best people I had met at Concordia. But despite that, right before the first day of class I thought to myself, “I am not qualified to be taking this class.”
Going over the syllabus was helpful, I saw the amount of discussions that were involved in the class and felt a little better. Reading papers was something that I enjoyed doing and learning more about real life applications of science sounded like a lot of fun. Neurochem was the first class that related what we were learning to things that were troubling the world. The things we knew, the things we didn’t know and everything in between. All too often students and people of Concordia say “BREW” but do not actively engage in the meaning of it. Becoming responsive engaged in the world. There are many ways to do, through Concordia’s five goals of liberal learning, and then beyond that as well.

Image source: https://itknowledgeexchange.techtarget.com/writing-for-business/writing-business-peak-peek-pique/
Meme source: me
This culmination of experiences is truly why Neurochemistry is the best class that I’ve taken at Concordia.

The neurochemistry capstone course offered a wide range of new subjects for me. It featured an outstanding group of seniors and juniors that created many useful and applicable discussions about neurological diseases, as well as advice by about life. The core focus of this class being a capstone requires the active engagement with our liberal arts education in the Fargo-Moorhead communities. This resulted in working with the social work class, allowing for making new friends and connections at Concordia. I found the community action project(CAP) a beneficial and powerful experience, showing the potential for students to collaborate to serve a better cause and attempt to solve some of the challenges encountered during our in class discussions.
I found the design of this class very beneficial, since many of the topics covered feature no direct answers, only more questions this resulted in open ended discussions. The open ended discussions allowed us to take components from our previous classes, and apply that knowledge in our search to find out more information on the research of the material. By teaching the class this way, it allows students to provide feedback during the discussions to each other, by seeing how each component of the research builds up to the larger picture of the disease. The ideas developed by each person in the class contributed to a greater understanding of the subject at the end of the week with our final discussions. The blog and wiki pages offered a meaningful resource for us to look further into our personal opinions, and express our thoughts to share them with the rest of the world.
The diversity of the different majors that compose this class offer a well rounded and this created lots of new friendships during the discussion of the topics. As the personal component to each of the discussions, is what drives us to seek more information about the diseases that effect us in our personal lives. During the ASD topic I found that very interesting and personal too, as growing up with a severely autistic sibling changed my views on the world, and this class allowed me to reflect with others and share what I have encountered and learned. This is what makes the class interesting, it isn’t another lecture that has no implications to you besides the next exam. The material learned during the class and discussions bears a personal connections that will stick with you for the rest of your life. You may not remember the exact pathways or molecules involved, though the exposure to the reality of the neurological problems provide potential outlets for many of us in this class to apply our content learned from our majors in future careers. As a majority of the students taking this class further plan to enter into the medical, research, pharmaceutical, and scientific industry that will help contribute small components to hopefully eventually help end these conditions. As that is the goal of the application of science, it serves as a means of knowing more about the world, and by acquiring as much information on these diseases is the first steps to solving them.
The CAP offered a meaningful and productive way of applying our understanding of neurological diseases and disorders. My project with mental health allowed our group to provide a better exposure of support structures and treatment options to college students on Concordia’s campus. As having known several close friends who have suffered greatly at college with their depression and anxiety, this make the issue personal to me. The impact of our project, and the discussion of the topic with other students showcased the need for better support networks for college students, and help to reduce the stigma of mental health issues. The challenges faced by the project and overcoming them provided a great sense of pride for me and my group members. I wish more classes offered more interconnected projects, as by working with other students from another field, showed what their goals and applicability of their major in solving real world problems.
The completion of this course is decisively a peak for my college experience, the open ended classroom provides a great environment for students to flourish in. It provides us with the basis of the ability for students to seek more than just the superficial components to a problem. The exams provided a better and more applicable means of solving complex problems from many small portions out of context. This class provides a direct link with our major and the serious issues that affect many people around the world. I am going to really miss this class, and all of the great individuals that are a part of it.
Tommy Styrvoky, class of 2019
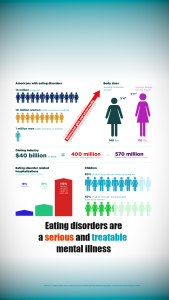
The implications of obesity have a rather large impact on our health system, as currently ≈40% of all Americans are obese, that results in 93 million people. This is brought about by our diets in America, as this results in a high fat diet and our sedentary habits only further make the problem worse. This results in a major cost issue for our medical system, as the current cost is estimated at around 147 billion dollars, and is estimated to increase another $48-$66 billion over the next two decades.
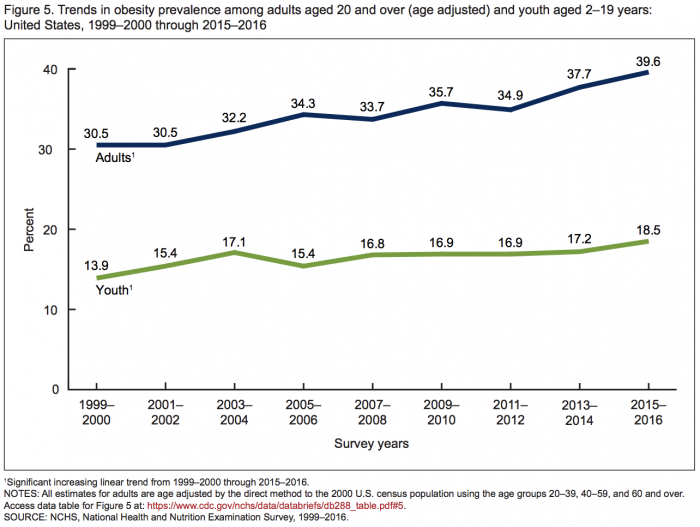
With the seen changes above, over the course of 16 years, a nearly 10% increase in obesity has occurred. There are many ideas as to why our body maintains an obese weight, however it is still dependent on your personal control of what you choose to ingest. As genetics plays a role in maintaining a set weight, but measures can be taken to adjust that weight. If done incorrectly, this results in a cycling of weight on and off around the set weight for an individual. The further implications of obesity can result in other serious health conditions, such as diabetes, heart disease, and hypertension.
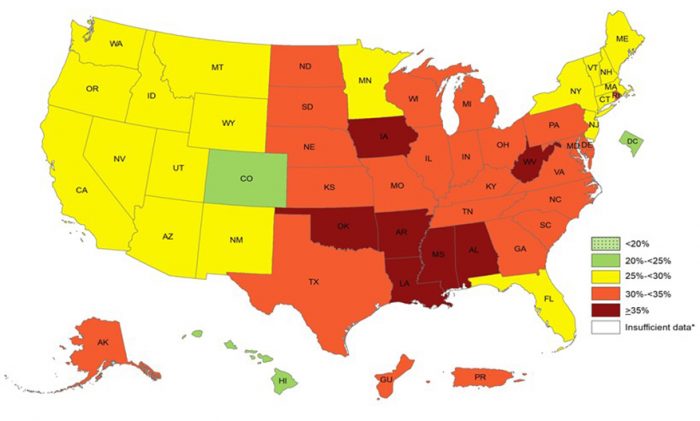
As seen on the heat map above, the south eastern portion of the US is at major risk for the obesity epidemic. There are several solutions to this, the first and easiest would be to change the dietary intake of processed foods, and try to eat foods that are lower in fats, sugars, and salts. The approach to this problem should be a personal one, if you can keep track of weight, and attempt to maintain or reduce your weight to a healthier weight by making your own food from healthy ingredients and trying to include more physical activity in your daily schedule.
https://www.huffpost.com/entry/us-obesity-2030-americans-obese_n_1893578

No path in life is straight and perfect. Not all answers are found in books or on the internet. The liberal arts education at Concordia College -Moorhead has allowed my shape of learning as “out of the box.” Various angles and approaches need to be taken when presented with a complex situation.
For all students grades create a very competitive and stressful environment. Grades are a very important part of any class because that is what is placed on the transcript. This class allowed for a non-stressful but well respected class. A majority of this class was participation, with two unique tests that challenged your thinking process and finally a project that took your own knowledge and present it in a form for others. Knowing that participation and willingness to learn allowed for less stress but with more want to become educated on these topics.
Articles that promoted learning
All the topics we had covered in Neurochemistry were more complex than I ever knew. We would start each week with an article that Dr. Mach had picked out. Each article was read by Monday along with a worksheet that asked for: main point in the article, a question to help explain a pathway or something super important that the article focused on, and finally, any questions you had. These papers all presented information that was new to all of us. Discussing the paper led to more questions than answers.
On Wednesday, we took all these questions and have posted our answers to the wiki page. Many times, I found that there was no new information. The question we had was said to be discovered but with an unknown function or was still being researched. We would either talk about our topic to the class or do this through “speed dating.” When conversing with classmates you started to see the connection between your topic and theirs.
Finally, on Friday all additional questions or comments that were talked about on Wednesday were discussed in groups. This day allowed for an open, no judgement discussion. Opinions were expressed and counter arguments peacefully.

Concordia’s five goals for liberal learning: