It seems that most colleges only test obedience. Students are presented information that they are supposed to obediently memorize, and then write it down on a piece of paper, which is graded. I do not find this to be helpful in preparing students for the world. Luckily, I attend a college where they have broken out of this mold. Concordia  College encourages liberal learning from the very first day you step foot on campus as a student. As freshmen are standing there wide-eyed in their bright yellow beanies, they are constantly reminded to “BREW.” If you are not from Concordia, I am assuming you are thinking of a different kind of brew. However, at Concordia, we understand BREW in a different context. To BREW means to become responsible engaged in the world. This concept is reinforced with Concordia’s five goals of liberal learning.
College encourages liberal learning from the very first day you step foot on campus as a student. As freshmen are standing there wide-eyed in their bright yellow beanies, they are constantly reminded to “BREW.” If you are not from Concordia, I am assuming you are thinking of a different kind of brew. However, at Concordia, we understand BREW in a different context. To BREW means to become responsible engaged in the world. This concept is reinforced with Concordia’s five goals of liberal learning.
Concordia has five goals for liberal learning:
- Instill a love for learning
- Develop foundational skills and transferable intellectual capacities
- Develop an understanding of disciplinary, interdisciplinary and intercultural perspectives and their connections
- Cultivate an examined cultural, ethical, physical and spiritual self-understanding
- Encourage responsible participation in the world
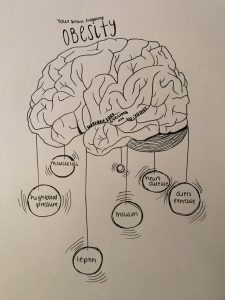
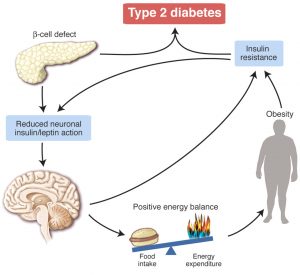
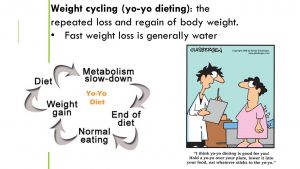
As I am wrapping up my capstone experience in Neurochemistry, I truly believe this course encompassed Concordia’s goals for liberal learning and what it means to BREW. But, before I tell you how these goals were met, I have to describe to you how this class worked because it was like no other class I have previously taken. Every week, we examined a specific article that dealt with a disease or condition that affected the brain, specifically the chemistry or signaling pathways, which was the underlying effect that caused the symptoms we superficially see.
Monday: we came to class with a general understanding of the research article of the week. Everyone read the given article over the previous weekend, and prepared answers to provided questions about the article. We were also asked to come with questions about the article. It was not hard to come up with questions, as most of these articles were very intricate and detailed. At the end of ever Monday, after discussing the article and gaining a better understanding of the literature, we, as a class, came up with questions that we wanted to explore to further better our understanding of the current article. We assigned ourselves to each question to answer for Wednesday.
Wednesday: we came to class after researching our question from Monday. Wednesdays were known as “speed dating.” There was an outer circle and an inner circle. The inner circle rotated after about five minutes of discussing your findings with the partner.
Friday: we had group discussions. The class was split into halves on and each half was led by a few of our fellow classmates. Fridays were always enjoyable because the group discussions were laid back and we talked about the article of the week in light of the actual world.

Every week, we incorporated what liberal learning is all about-
- Instill a love for learning.
Neurochemistry was all about self-learning. There was no textbook, no powepoints, nothing. The material you learned was through your own love and desire to learn. This is one thing that I loved about Neurochemistry. I would spend hours reading and vetting articles about the topics we covered, learning as much as I could.
- Develop foundational skills and transferable intellectual capacities.
Neurochemistry developed skills that I will use for many courses down the road, hopefully in medical school. For example, reading scientific literature takes practice to fully understand. The learning in this course, from my experience, was from scientific literature because the diseases and conditions we discussed are all topics of intense current scientific research. The second half of this goal references “transferable intellectual capacities.” I perceive this as not only using the information in the course in other intellectual capacities, but also transferring your own knowledge in a manner in which other people can understand. This was a major topic in neurochemistry. We spent a lot of time trying to effectively communicate our findings to the rest of a class. This is a challenge because most people get bored or tune out scientific talk/jargon. Therefore, this class was very beneficial in ways that I can use to talk about science with people who do not have a scientific background.
- Develop an understanding of disciplinary, interdisciplinary and intercultural perspectives and their connections
Neurochemistry can be applied to many other areas of science and the world. One of my favorite sayings, which comes from a Time magazine I read back from when I was around 5th grade, is “you are your brain.” This phrase has stuck with me and it seemed extremely relevant in neurochemistry. So, because we are our brains, and this course was learning about the chemistry and signaling of the brain, I believe this course touched on nearly every scholarly disciplinary. There is not one subject in school that I can think of that does not have a neurochemistry undertone.
- Cultivate an examined cultural, ethical, physical and spiritual self-understanding
During our group discussions on Fridays, which were my favorite, we often discussed how our western lifestyle seemed to be an underlying factor for how our brains were altering. We examined ethics of certain medications, or one Friday we discussed the implications of physician-assisted suicide for patients with terminal illnesses such as ALS. This was a somber and heavy discussion, but it is a real-world issue nonetheless. We talked about death, and sometimes our own religions compared to others and what that does for our belief-system.
- Encourage responsible participation in the world
Lastly, our capstone project allowed us to reach out to the Fargo/Moorhead community. Personally, I was apart of the autism group. Our group decided to offer a student workshop that was geared toward education majors and working with students with autism as well as their parents. Although we had challenging times trying find a speaker, it all worked out as we found a fantastic person who fit our project perfectly. We worked with a mother who has a child with autism, and the experience was very humbling. The rest of the groups of our class had their own projects that acted with or for the community. Our projects actually helped people, they were not just presenting information to other students who are probably not paying attention anyway.
Ultimately, neurochemistry encompasses what it means to be a Cobber. As a Cobber who is graduated in the spring, we are constantly reminded to BREW- become responsibly engaged in the world. This is exactly what we did during my capstone experience. At Concordia College, and through this capstone experience, we are taught a much larger aspect than just grades. I know that as I leave Concordia with my diploma, I will be ready to BREW.


 College encourages liberal learning from the very first day you step foot on campus as a student. As freshmen are standing there wide-eyed in their bright yellow beanies, they are constantly reminded to “BREW.” If you are not from Concordia, I am assuming you are thinking of a different kind of brew. However, at Concordia, we understand BREW in a different context. To BREW means to become responsible engaged in the world. This concept is reinforced with Concordia’s five goals of liberal learning.
College encourages liberal learning from the very first day you step foot on campus as a student. As freshmen are standing there wide-eyed in their bright yellow beanies, they are constantly reminded to “BREW.” If you are not from Concordia, I am assuming you are thinking of a different kind of brew. However, at Concordia, we understand BREW in a different context. To BREW means to become responsible engaged in the world. This concept is reinforced with Concordia’s five goals of liberal learning.