You’ve hit your head, so what? Now you have a little headache, no big deal right? Wrong. Chances are if you experience a headache along with symptoms such as sensitivity to light and sound, along with issues concentrating after hitting your head, you have a concussion.
What is a concussion?
Most people, refer to a concussion as a brain bruise. This trauma to the brain is more than a little bruise. When a person’s head is hit, their brain sloshes around in their skull. Depending on the angle, and the force of the hit the concussion can range from mild, to severe or traumatic. The initial sloshing of the brain leads to an influx of ions in between different neurons. This abnormal activity between neurons leads to the activation to an immune response, and as a result histamine is released. This release of histamine results in inflammation, which in turn results in oxidative stress. This stress on the brain leads to the build up of toxic proteins which leads to cell death.
When a concussion happens, the membrane of the brain stretches there is an efflux of potassium, and an influx of calcium in the neurons. The rapid influx of calcium ions leads to excitotoxicity. At the same time there is an increase of glucose metabolism, and an increase in ATPase activity as the brain tries to get back to homeostasis. This hypermetabolism leads to increased protease activation. As the cascade of a concussion continues to happen the cell begins to run low on energy trying to fix all the problems that are simultaneously occurring. This leads to an energy crisis, and the neurofilament side-arms can now be phosphorylated which leads to the collapse of the axons. This collapse of the axons causes microtubule disruption, which in turn diminishes the normal signaling between neurons and the rest of the body.
Classification of TBIs and Recovery
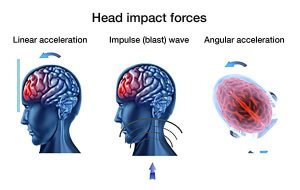
Like people, no two concussions are the same. Depending on the force of the hit, and the location and area of the hit the class of the concussion changes. There are two main classes of traumatic brain injuries or TBIs.
- Mild
- Severe
Mild, have a faster recovery time than severe, and the symptoms displayed are less.
Studies have shown, that it takes adults 10-14 days to recover from a mild TBI, and children 18 and under take about 4 weeks to recovery. Of course, recovery time depends on the person and the severity of the concussion. There are five steps to recovery from a concussion.
- Acute Injury: This is the first 72 hours after a concussion. There may be some testing done at this step like the ImPACT test. During this time symptoms may evolve and change during this time.
- Initial Rest and Recovery: Initial testing such as the ImPACT test, a balance test, and a neuropsychology test, may be done at this time, and if necessary a care plan is created.
- “Hunker Down”: During this phase some days are worse than others, but in order to recovery in a healthy manner, you should take recovery a day at a time.
- Mountaintop: At this stage symptoms are mostly resolved, however, you should still take care to not go back to full exertion
- Transition: In this stage symptoms are gone. You can now resume all activities, and no longer worry about the TBI.
More than a bruise
If someone you know has experienced a concussion, and is slow to return back to “normal” remember….
A concussion is more than a bruise. Every time a concussion occurs the normal functions of the brain are disrupted. Additionally, each subsequent concussive event causes more damage than the previous one. Studies have shown that suffering from multiple concussions can leave you at a higher risk for, anxiety, depression, and Alzheimer’s Disease.
Images:
Image 1: https://crls.cpsd.us/athletics/sports_related_head_injury_and_concussions
Image 2: https://www.headsmart.me/
Image 3: https://concussionu.wordpress.com/concussion-management/

 familiar with the initial symptoms associated with concussions like headaches, memory issues and sensitivity to light; however, there are chemical changes happening in the brain to cause these symptoms and can explain long term changes that happen to one’s brain after a concussion.
familiar with the initial symptoms associated with concussions like headaches, memory issues and sensitivity to light; however, there are chemical changes happening in the brain to cause these symptoms and can explain long term changes that happen to one’s brain after a concussion. rest is the best way for one’s brain to recover from a concussion. This entails resting both physically and mentally which may include eliminating screens, reading, working and driving for a certain amount of time.
rest is the best way for one’s brain to recover from a concussion. This entails resting both physically and mentally which may include eliminating screens, reading, working and driving for a certain amount of time.
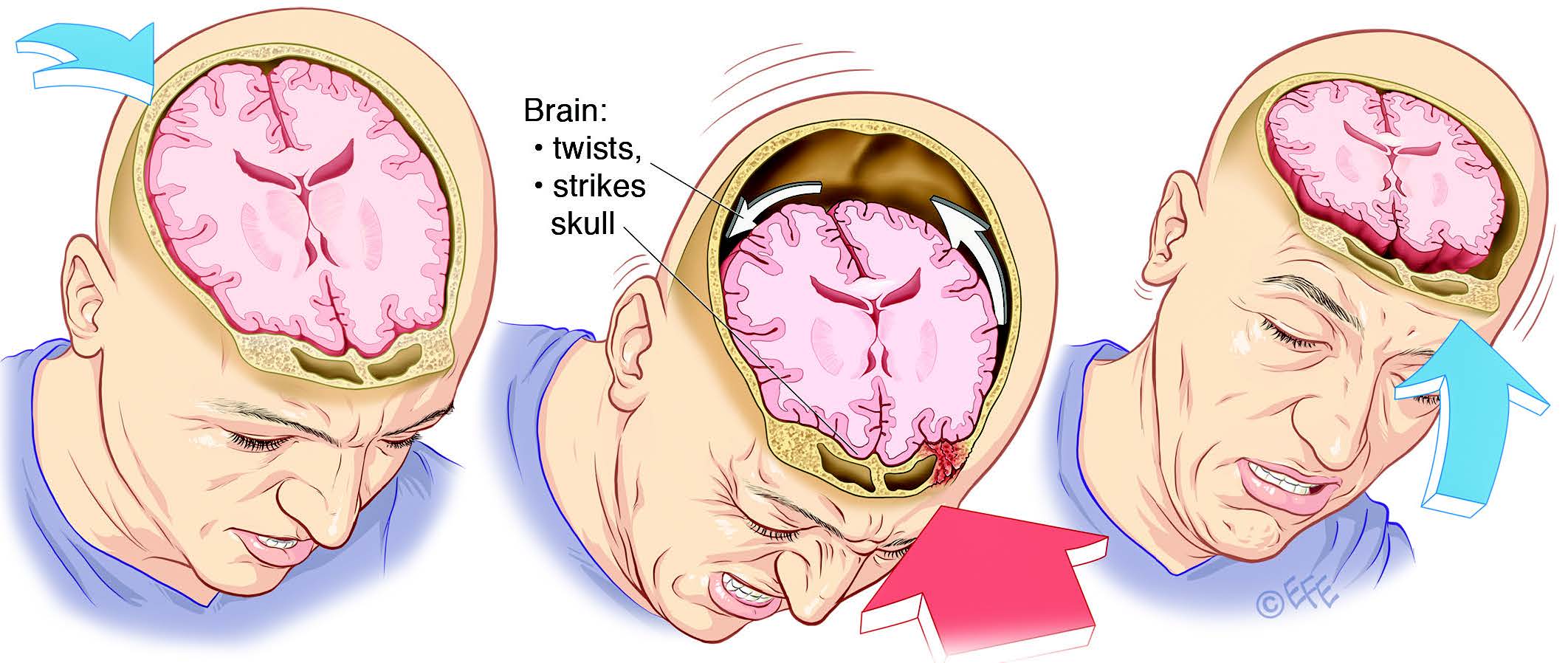

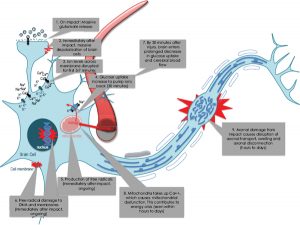





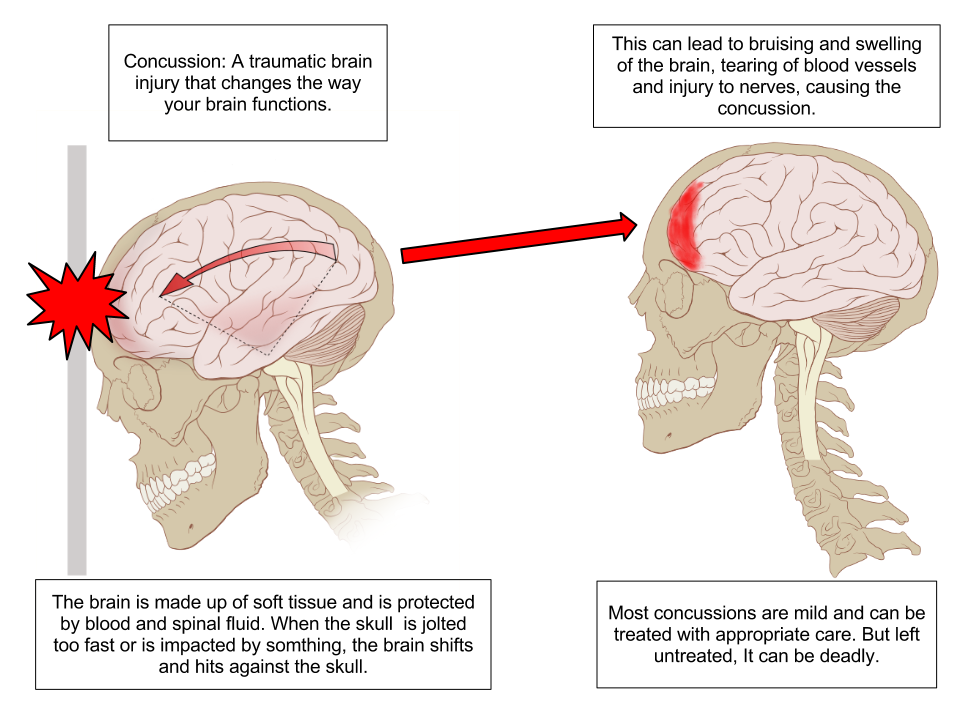 possible skull deformation. Depending on the force, position and angle of contact,concussions can vary in severity and symptoms. Typical symptoms stem from a cascade of molecular events inside the brain that shift from normal function. Balances of major ions in the brain like potassium, glutamate, and calcium are shifted during concussions, requiring energy in the form of ATP to return to homeostasis. This in turn calls for an influx of glucose to provide the ATP to the
possible skull deformation. Depending on the force, position and angle of contact,concussions can vary in severity and symptoms. Typical symptoms stem from a cascade of molecular events inside the brain that shift from normal function. Balances of major ions in the brain like potassium, glutamate, and calcium are shifted during concussions, requiring energy in the form of ATP to return to homeostasis. This in turn calls for an influx of glucose to provide the ATP to the cell. After this initial influx in ATP and glucose, there is a depression of both compounds following concussion. The development of free radicals is also a result of concussion, causing damage to DNA and other fragile cell material. Other effects of concussion include damage to axons, synaptic plasticity, and connectivity changes.
cell. After this initial influx in ATP and glucose, there is a depression of both compounds following concussion. The development of free radicals is also a result of concussion, causing damage to DNA and other fragile cell material. Other effects of concussion include damage to axons, synaptic plasticity, and connectivity changes.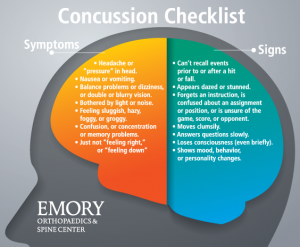 While there is no way to stop the cascade resulting from concussions, symptoms can be regulated with plenty of rest and reduced stimulation. Staying away from screens and intense reading can increase the recovery speed, and help alleviate symptoms like headache and difficulty focusing on things. Rest in this case means not doing things that exacerbate symptoms
While there is no way to stop the cascade resulting from concussions, symptoms can be regulated with plenty of rest and reduced stimulation. Staying away from screens and intense reading can increase the recovery speed, and help alleviate symptoms like headache and difficulty focusing on things. Rest in this case means not doing things that exacerbate symptoms Over fall break this year, I had the opportunity to travel to North Carolina to visit the
Over fall break this year, I had the opportunity to travel to North Carolina to visit the  The experien
The experien All things considered, society needs to start taking concussions more seriously–it is a brain injury, after all. We tend to think that it is more important to return to playing a sport or return to class than it is to properly care for a concussion. I personally have had experience with a few concussions. Specifically, sophomore year, I was involved in an accident that resulted in a major Traumatic Brain Injury (TBI). I lack any memory for months following the event. The one memory I do have is of sitting in class, about a week post-injury, and trying to take notes. I was nauseous, dizzy, and close to passing out. I had to leave class because I felt so sick. When I looked back on those notes a few weeks later, they were merely scribbles and random lines. I then realized that I should not have forced myself into going back to class so soon. I needed the rest. But society values us for our productivity, whether academically or athletically. When that “go go go” mentality is ingrained in us, it becomes hard to step back and take care of ourselves. This needs to change. Major TBIs and frequent head injury can lead to issues with mental health, cognition, memory, and neurodegenerative disease such as CTE. Just like we would take care of a broken leg, we must take care of our brains.
All things considered, society needs to start taking concussions more seriously–it is a brain injury, after all. We tend to think that it is more important to return to playing a sport or return to class than it is to properly care for a concussion. I personally have had experience with a few concussions. Specifically, sophomore year, I was involved in an accident that resulted in a major Traumatic Brain Injury (TBI). I lack any memory for months following the event. The one memory I do have is of sitting in class, about a week post-injury, and trying to take notes. I was nauseous, dizzy, and close to passing out. I had to leave class because I felt so sick. When I looked back on those notes a few weeks later, they were merely scribbles and random lines. I then realized that I should not have forced myself into going back to class so soon. I needed the rest. But society values us for our productivity, whether academically or athletically. When that “go go go” mentality is ingrained in us, it becomes hard to step back and take care of ourselves. This needs to change. Major TBIs and frequent head injury can lead to issues with mental health, cognition, memory, and neurodegenerative disease such as CTE. Just like we would take care of a broken leg, we must take care of our brains. 





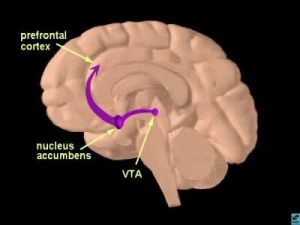 The human brain is capable of many complex memories and emotions all driven by chemical interactions and signaling in distinct brain regions. In response to experiences like eating food, sleeping, or having sex a portion of the brain called the reward pathway is activated. This pathway creates lasting memories connecting certain activities with the feeling of reward and encouraging repetition of the behaviors. Activation of this pathway takes place in the ventral tegmental area (VTA) which projects to the nucleus accumbens (NAc), with signals propagated by the release of the neurotransmitter dopamine. Dopamine creates the feelings of euphoria and energy and function to remind our brains to do things that help us survive.
The human brain is capable of many complex memories and emotions all driven by chemical interactions and signaling in distinct brain regions. In response to experiences like eating food, sleeping, or having sex a portion of the brain called the reward pathway is activated. This pathway creates lasting memories connecting certain activities with the feeling of reward and encouraging repetition of the behaviors. Activation of this pathway takes place in the ventral tegmental area (VTA) which projects to the nucleus accumbens (NAc), with signals propagated by the release of the neurotransmitter dopamine. Dopamine creates the feelings of euphoria and energy and function to remind our brains to do things that help us survive. However, when addictive drugs are involved in this brain circuitry and dopamine levels are unnaturally raised the reward pathway is overthrown. A large euphoric high along with the connection of drug using behaviors with the reward leads to what we know as addiction and drug seeking behaviors. Addictive drugs act in different ways in the brain, but all function to make more dopamine available to activate the neurons in the NAc and signaling to the frontal cortex.
However, when addictive drugs are involved in this brain circuitry and dopamine levels are unnaturally raised the reward pathway is overthrown. A large euphoric high along with the connection of drug using behaviors with the reward leads to what we know as addiction and drug seeking behaviors. Addictive drugs act in different ways in the brain, but all function to make more dopamine available to activate the neurons in the NAc and signaling to the frontal cortex. The stress pathway can add to the dopamine levels in the reward pathway and compound drug-seeking behaviors in addiction. The release of dopamine driven by glucocorticoid hormones functions to increase the euphoric sense and desire to return to the behavior triggering the reaction. In an experiment done on rats addicted to cocaine, after being given a small amount of cocaine as a trigger, rats with excess stress hormones or an external stressor showed more signs of relapse than those that did not have increased stress levels.
The stress pathway can add to the dopamine levels in the reward pathway and compound drug-seeking behaviors in addiction. The release of dopamine driven by glucocorticoid hormones functions to increase the euphoric sense and desire to return to the behavior triggering the reaction. In an experiment done on rats addicted to cocaine, after being given a small amount of cocaine as a trigger, rats with excess stress hormones or an external stressor showed more signs of relapse than those that did not have increased stress levels.