Imagine sitting at your desk in your bedroom while trying to hurriedly finish up your homework that is due tomorrow. While focusing intensely on a problem, you begin to hear whispering. Thinking that it is just a result of the silence in your room mixed with exhaustion from studying all evening, you brush it off even though the whispering persists. After you get ready for bed and are lying still trying to fall asleep, the whispering seems to get louder and you cannot help but feel as though someone is there whispering into your ear. You want to speak out to the whispering, but feel confident that there is no one there.

This could be just one symptom of schizophrenia, as auditory hallucinations are the most common type of hallucination occurring for most people with schizophrenia. There are many other symptoms, including:
- delusions
- disorganized thinking or speech
- disorientation
- memory loss
- disorganized behavior
- abnormal motor behaviors
- speech issues
- lack of ability in various areas
The cause of schizophrenia creates a difficult conversation, as there are many different theories. However, most theories conclude that schizophrenia is caused by some type of genetic predisposition combined with environmental factors that allow the affected genes to become expressed. There are also risk factors that can increase the likeliness of developing schizophrenia, including:
- family history of schizophrenia
- increased immune system activation
- being born with older parents
- some pregnancy and birth complications
- taking mind-altering drugs during teens
Some of the risk factors for schizophrenia correlate with the environmental factors that can also increase the development of schizophrenia:
- childhood trauma
- prenatal risks
- migration
- place of birth
- infections
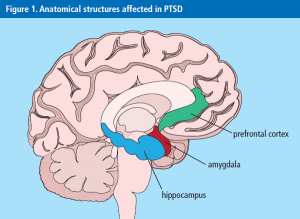
When looking at how schizophrenia occurs in individuals, it is often a misconception that these individuals are in control of their symptoms and actions, causing them to be stereotyped against in society. The true cause of schizophrenia is located in the brain and in many different brain regions. The brain regions that are most affected and involved in schizophrenia are:
- gray matter
- dorsolateral prefrontal cortex
- inferior prefrontal cortex
- medial temporal cortex
- primary auditory cortex
- visual cortex
- auditory language regions such as Wernicke’s area and Broca’s area
- basal ganglia

When seeing the number of brain regions involved in schizophrenia and how they impact the symptoms most generally exhibited, it becomes clear that schizophrenia is a much more genetic based condition and although influenced by environmental factors, is definitely not directly caused without any type of genetic influence.
As previously discussed, the treatment of schizophrenia is a tricky one and there are constant developments in the best and most effective ways to treat individuals with schizophrenia. The most common ways used today are medication and psychosocial treatment, with many people with schizophrenia requiring frequent visits with a psychiatrist. Below is a link to a video of an emerging finding of a schizophrenia “switch” and how it may impact treatment:
https://www.youtube.com/watch?v=m6YE6BJVwtg
The lifestyle of someone living with schizophrenia can be very difficult and often comes with many judgements and obstacles. First, finding the correct combination of medication for individuals with schizophrenia is a very long and difficult journey and can be extremely expensive and tasking on the individual, especially if the medication does not work immediately or is the wrong combination and the symptoms are not controlled. Second, most people in the general population have preconceived stereotypes about those with schizophrenia based on what they have heard, what they have understood from others, or what they have seen in media. Finally, managing symptoms with or without medications for individuals with schizophrenia is very difficult and their symptoms often arise without notice and in unexpected ways.
http://2018neurochem.pbworks.com/w/page/129829617/Wnt%20and%20Schizophrenia


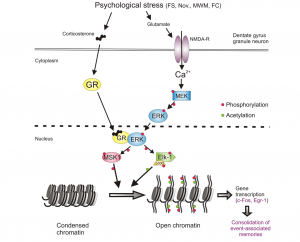
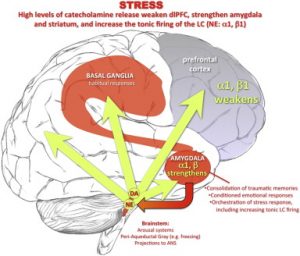 weakened, such as the prefrontal cortext. The amygdala is opposite. Because this part of the brain consolidates so many of these traumatic memories, when the memories are triggered, the amygdala springs in to action.
weakened, such as the prefrontal cortext. The amygdala is opposite. Because this part of the brain consolidates so many of these traumatic memories, when the memories are triggered, the amygdala springs in to action.



 udy showed that participants who exercised responded better to stress, increasing the levels of GABA as opposed to the participants who did not exercise3. Seek advice from a doctor if anxiety seems too much to bear. However, maybe the only prescription someone needs in order to feel less anxious is to exercise more! GABA levels increase with more exercise, diminishing the activity of neurons that lead to anxiety; thus, calming the hippocampus. Maybe, all you need to do is just sweat out the anxiety.
udy showed that participants who exercised responded better to stress, increasing the levels of GABA as opposed to the participants who did not exercise3. Seek advice from a doctor if anxiety seems too much to bear. However, maybe the only prescription someone needs in order to feel less anxious is to exercise more! GABA levels increase with more exercise, diminishing the activity of neurons that lead to anxiety; thus, calming the hippocampus. Maybe, all you need to do is just sweat out the anxiety.