What is autism and why does it matter?
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by challenges in social communication and restricted, ritualistic or repetitive behaviors. As a spectrum disorder it varies greatly in the type and severity of symptoms the individual experiences.
ASD has three categories, broken down by how severe the diagnosis is: high-functioning, autism, and severe autism. One key thing to note however is that a person can fluctuate in their location on the spectrum throughout time as it is not a rigid system and they continue to grow and develop.
This disease continues to become more and more prevalent as years go on. 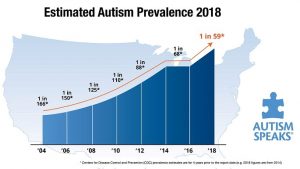 In a 2014 study done by the CDC’s Autism and Developmental Disabilities Monitoring Network it was found that about 1 in 59 children were identified to have ASD, an increase of 15% since the two-year prior 2012 study. With this prevalence on the rise researchers have begun trying to find a link that will explain ASD and how it has multiple, perhaps interlocking, causes.
In a 2014 study done by the CDC’s Autism and Developmental Disabilities Monitoring Network it was found that about 1 in 59 children were identified to have ASD, an increase of 15% since the two-year prior 2012 study. With this prevalence on the rise researchers have begun trying to find a link that will explain ASD and how it has multiple, perhaps interlocking, causes.
So, what do we know?
Autism is at least in part genetic.
We know there is a genetic factor by looking at the concordance rate within families, the probability that if one sibling has autism another in the family will also have autism. For identical twins this value is 77%, in fraternal twins it lies at 31%, and regular siblings are around 20%. What we learn from these numbers is that it accounts for a lot of the risk but not all of it. Identical twins do not hold 100% so it cannot be solely genetic. Environmental factors come into play with the fraternal twins, holding the similar but not same genetic coding but sharing the same environment, at 31% but regular siblings at 20%. An 11% difference due to the shared environment.
It’s been found that there are over 1,000 identified genes linked to autism we cannot say one single gene causes it due to its spectrum. It may be one gene for one child/ family but a combination for another, each case is different. We are starting to group them together by their roles and pathways. Genetic mutations play their own role adding in to the overall problem and each case will have different ones, this is how it was not passed genetically from the parents but was created within the child.
The genes involved tend to code for proteins that regulate gene transcription, excitatory/ inhibitory signaling, and overall brain development. These mutations can be a due to a change or lack of single letter, an entire section or even the entire gene leading to profound effects on the brain. These include location errors of the neurons leading to altered morphologies and malformation, dysregulation of development commonly involving plasticity, maintenance, autophagy which is the body’s ability to consume its old or unnecessary cells, and much more.
Autism is at least in part caused by environment.
We know that while the fetus is growing and developing, especially during brain development, it is very vulnerable and susceptible to different agents. Exposure to some of these agents increase the risk of autism. It was found that mothers who were diagnosed with two or more infections during pregnancy were at a higher risk of having a child with autism than those with one. Certain infectious agents themselves can also cause autism.
Problems in the immune system, especially regarding inflammation and abnormalities, have shown links to autism as well. Autistic children are more likely to have inflamed areas of the brain in addition to having denser, more neuronal regions as well. This is due to different pathways being nonfunctional such as autophagy which cleans up old and nonrequired neurons for the generation of better connections.
Some of this is even more prevalent due to zinc deficiencies as many components of the immune system require zinc to function properly. Without a properly functioning immune system the CNS won’t develop regularly. Immune responses can vary greatly, however with improper regulation autistic brains have reduced ability for knowing when to stop which leads to inflammation and damage within the brain.
Overall, autism is a very complex disorder with multiple causes likely interconnected. We are simply barely below the surface of what is all involved from genetic to environmental components. As more research comes out we are able to understand this disorder better and keep adding pieces to the puzzle that is autism.




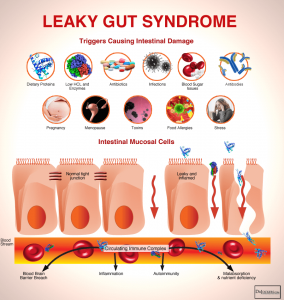




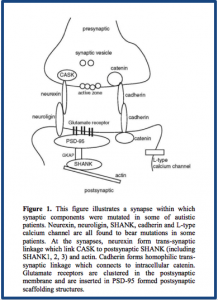



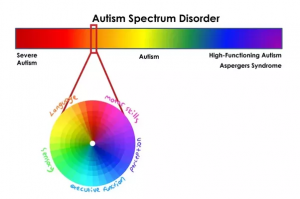
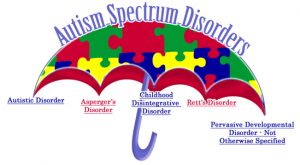

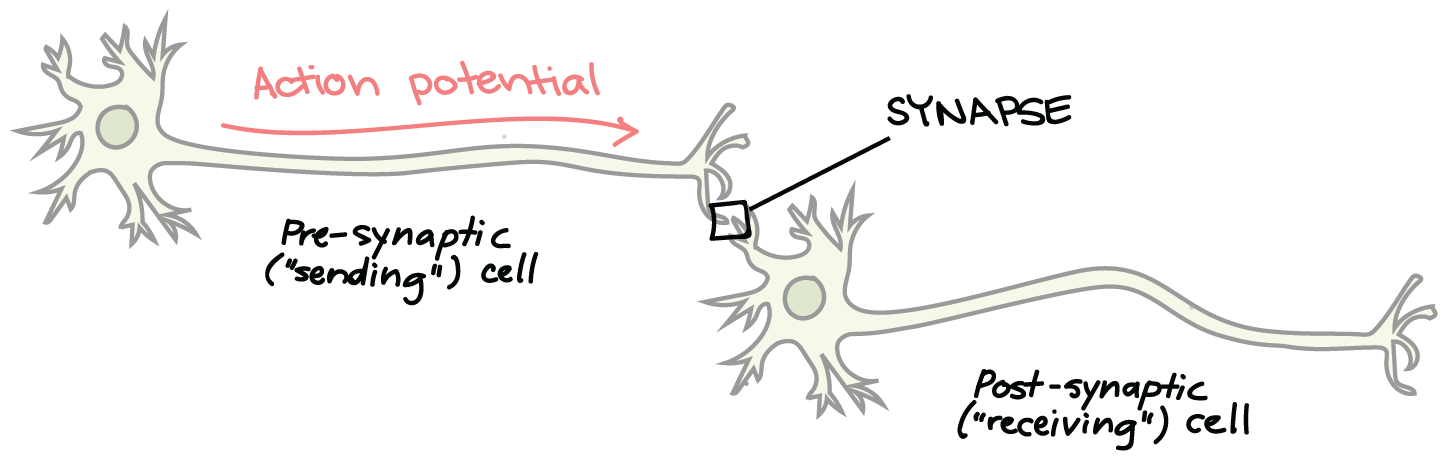 Fig.
Fig.