35% of adults age 20+ are obese. This is becoming a severe problem, especially in the United States. What is causing this spike in obesity? How does obesity become an issue in the body? I would like to discuss the background related to this topic.
Inflammation and obesity:
The issue with obesity usually begins with the body becoming insulin resistant. The resistance is caused by overnutrition. Overnutrition or overeating causes stress in the body, particularly in the organelles like the mitochondria and the endoplasmic reticulum which are devoted to breaking down the foods we eat and creating proteins in the body. In overnutrition, these organelles become overwhelmed which leads to activation of the JNK pathway. This is a pathway normally implicated in the stress response, therefore, it acts to inhibit the insulin receptor substrate and causes inflammation. This in turn leads to more inflammation and more shutting down of the insulin receptor and insulin receptor substrate.
Insulin Resistance:
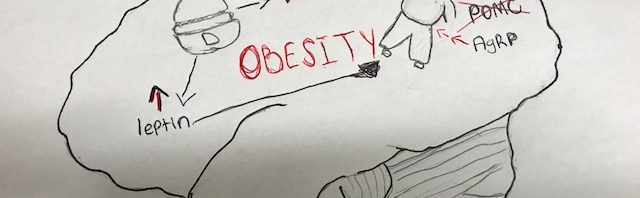
The shutting down of the insulin receptor and insulin receptor substrate makes it increasingly hard for insulin in the body to do its job. Normally, when we eat food, insulin is released in the body and it signals POMC and AgRP neurons in the hypothalamus which tell the body to stop eating. However, in overnutrition the shutting down of receptors causes the body to not react to the insulin being released. The beta cells in the pancreas are responsible for making insulin and as insulin resistance begins they are able to make increasing amounts of insulin to try to combat the resistance. However, at some point a threshold is reached and the body cannot produce enough insulin. This leads to hyperinsulinemia and usually the onset of type 2 diabetes.
Onset of obesity:
Eventually, the insulin is not sufficient to produce a response in the body. Therefore, the body cannot recognize that you’re consuming too much food and will constantly signal to keep eating. The stress continues and just potentiates the problem and causes obesity. This is just some of the pathology behind obesity. With the excess of food and availability of food that we have now, it helps to explain the reason why obesity is such a problem right now. Finding a solution is increasingly important as obesity and type 2 diabetes have very negative impacts on the body.

Onset of Obesity from: http://www.life-enhancement.com/images/LEM1211chart211.gif
For more information about obesity and its pathology read:
https://moodle.cord.edu/pluginfile.php/625315/mod_resource/content/0/2013%20CNS%20insulin.pdf
Featured image from:
https://d2s9xe8pzxi1js.cloudfront.net/wordpress/wp-content/themes/Marks-Daily-Apple-Responsive/images/blog/obesitycrisis.jpg
Science & Stigma With Obesity
Obesity is a common and serious health issue in the United States. According to the CDC, more than 1/3 of US adults have obesity and it’s on the rise. Obesity puts someone at a higher risk of heart disease, stroke, type 2 diabetes, and certain types of cancer. So why is this such a rising issue and what is really happening biologically with obesity?

Obesity Science
Normally, when we eat food, there are two types on neurons in our brain that regulate our appetite. POMC-neurons tell us to stop eating and AgRP-neurons tell us to eat. Eating causes release of the hormone insulin, which activates POMC-neurons to get us to eventually stop eating. However, when obesity is present, we eat too much. This over eating causes our neurons to become stressed and overworked, which makes the normal insulin regulation work incorrectly. The POMC-neurons are unable to tell us to stop eating and the AgRP-neurons are over activated. This in combination with the reward system of our brain that responds positively to our favorite foods is no match for any sort of will power anyone may be able to muster.

Rethinking Obesity
Society paints this picture of obesity as this condition people have because they have no self-control around food and are lazy, living a sedentary life. This however isn’t the case for most people suffering from obesity. Obesity is a biological disease that effects how our brain functions. Take that in combination with many of the foods and food additives present in our society not being healthy and adding to the problem, basically a person is helpless against all odds. Treatment for obesity can be a lifestyle change, but also may require medication or surgery to reset the neurological imbalance that is present. As research into obesity continues, maybe we’ll be one step closer to finding effective treatments and even preventative treatments for obesity.
For more on the science behind obesity: www.sciencedirect.com/science/article/pii/S1043276012002044?via%3Dihub
Feature Image: https://www.medicalnewstoday.com/articles/317546.php
Obesity aspects image: https://www.learnhowtobecome.org/make-a-difference-careers/obesity/
Food friends image: https://www.oyewiki.com/health/obesity-a-friend-or-an-enemy-6-9-2017
Why You Should Think Twice Before You Sign up for a Gastric Bypass
Gastric bypass has gotten very popular in the recent years since it promises easy results. Just like everything that comes easy, it has a price. The gastric bypass procedure was made for people who are extremely obese (BMI 40 and above) or have very complex weight related problems with a BMI of 35 or above.
BMI is used as a general guideline to see how people compare to people with similar sizes. For example:
Underweight, BMI 18.5
Healthy weight, BMI 18.5-24.9
Overweight, BMI 25-29.9
Obese, BMI 30 and above
Once a patient reaches the obese category, the patient has higher risk of diabetes, high blood pressure, and other cardiovascular problems. Gastric bypass was made to help patients in that situation to help get out of it, since the issue of over eating can tend to be due to a discrepancy within the neural pathway.
What is gastric bypass?
It is a procedure where the stomach is cut significantly smaller making less room for food and connected into the small intestine. So, for a patient to eat a full meal with a small stomach like that is difficult make the patient feel full faster causing them to lose weight. But this isn’t just solving the space issue within the stomach but also causing inhibitory signals to the brain to increase letting that person feel full faster. After a while the patients usually are able to eat a little more but the lower number of cravings and the small stomach space restricts them from over eating.
This does seem like a harmless and easy solution, but it should only be performed for patients who are at a very high risk of
The Other Side of Obesity You Did Not Know
If you went around asking people what they think the cause of obesity is, they will most certainly tell you it is overeating. Even though they are right, they usually ignore other factors that lead to obesity. The notion that obesity is a disease is still not well accepted by the public. In this blog I will try to demonstrate how other factors can put a person at a high risk of being obese.
But before we dig into the all sciencey stuff we have to understand what obesity is.
What is obesity?
Obesity is excess adipose (fat) tissue. What is this, you ask? So a fat cell is an endocrine cell and adipose tissue is an endocrine organ. Significantly, excess adiposity or obesity causes increased levels of circulating fatty acids and inflammation. You can look at obesity as excessive body fat.
So how do I know if am obese?
Excess fat tissues can be determined by the use of a Body Mass Index (BMI). BMI is a mathematical calculation involving height and weight, irrespective of family history, gender, age or race. BMI is calculated by dividing a person’s body weight in kilograms by their height in meters squared (weight [kg] height [m] ^2) or by using the conversion with pounds (lbs) and inches (in) squared.
Other factors to known.
Insulin: we usually associate insulin with low blood sugar and diabetes. Most people know that the role of insulin is to regulate metabolic processes like glucose uptake and lipid synthesis. What they don’t know is that insulin and insulin signaling plays a big role in obesity. Insulin acts on two neurons in the brain.
- The POMC neurons which signals us to stop eating
- The AgRP neurons which signals us to eat
But what happens is
- Over nutrition leads to
- Hyperinsulinemia (too much insulin)
- Which leads to insulin resistance
- That causes inhibition of the POMC neurons that tell you to stop eating
- Leaving the AgRP neurons that do not tell to stop eating so you over eat
Leptin: Leptin is a hormone that is produced by the fat cells in the body. Its main role is regulating how many calories we eat and burn, as well as how much fat we carry on our bodies. The more body fat they carry, the more leptin they produce. What happens is that,
- Eating->Increased body fat->Increased leptin->Decreased appetite, increased energy expenditure
But in leptin resistance, leptin does not signal to the brain that we are full and so we keep eating.
- Overeating ->increases body fat-> increased leptin( too much this time)-> blockage of signaling to the brain -> obesity
And just a reminder, obesity is not joke. It puts individuals at risk for more than 30 chronic health conditions. They include: type 2 diabetes, high cholesterol, hypertension, gallstones, heart disease, fatty liver disease, sleep apnea, GERD, stress incontinence, heart failure, degenerative joint disease, birth defects, miscarriages, asthma and other respiratory conditions, and numerous cancers. Think twice before you eat that box of pizza for a second time in a week.
Obesity: More Than Meets the Eye
Obesity rates are skyrocketing, and there is no denying that it is a large problem for our country. There are many contributing factors that lead to the development of obesity. As our diets has become more and more heavily composed of fat, sugar, and carbs, our bodies are undergoing changes that are leading to extreme health problems, including Type 2 diabetes and Obesity. Processed foods have become more addictive, because of the high amounts of fat, sugar, and additives they contain. These components in our food are altering the normal signaling within our bodies, leading to the development of chronic metabolic illnesses.
The Role of Insulin
Insulin is a key factor that our bodies use in maintaining energy homeostasis. Insulin is used to regulate the amount of energy your body needs and expends.
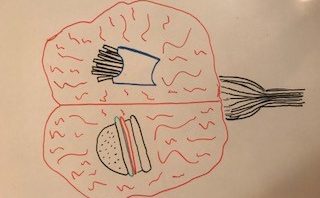
After we eat, insulin is released into the bloodstream, causing the food (glucose) that we consumed can be absorbed into our cells and used for energy. Insulin also acts in the brain where it binds to its receptors on neurons in the hypothalamus, causing an anorexigenic response. The anorexigenic response is one that lets you know you are full and should stop eating.
Insulin and Reward
Insulin also acts on dopaminergic neurons in the midbrain (involved in the reward pathway) The desire to eat is not only driven by the body’s current nutritional state, but also by the rewarding aspect of food. Reward- based eating behavior is likely linked strongly with obesity because the signaling in these circuits can eventually override the signaling in the hypothalamus. Insulin is able to change reward-related behavior by decreasing sucrose intake and conditioned preference for high-fat food. Therefore, insulin signaling is involved with the regulation of energy homeostasis and food intake in these neurons as well. When fed, insulin signals for you to stop eating for pleasure, and attempts to control your food intake.
Insulin Defects= Bad News
Eating a high saturated fat diet causes disruptions in the insulin signaling pathway, thus interfering with energy homeostasis and the sending of messages to stop eating. This leads to inflammation in the brain and causes lots of stress in the cells. A cascade of inflammation begins; making the insulin receptor unable to continue the cascade that is supposed to occur once insulin is bound. This particular problem is what is known to be Type 2 diabetes. Insulin is present, and so is its receptor, but the rest of the pathway is dysfunctional.
Effects of Processed Foods
Since processed foods contain fat and sugar than we are not meant to consume, when we them, we start to crave them because the chemicals, fats and sugars they contain are causing chemical changes in our brains. This can lead to insulin resistance and the dopamine reward pathway can eventually override the hypothalamus, since we develop such a strong desire to eat these foods. It is a cascade that can very quickly get out of control and manifest into what is essentially brain disease, presenting itself visually as obesity.
Treatment
Hedonic feeding, the term used to describe the drive to eat to obtain pleasure, without actually having an energy deficit, is the type of hunger that most weight-loss programs are targeting. They are focused on relieving cravings, instead of targeting the hypothalamus and the inflammation/stress that occurs there due to the insulin resistance that occurs. There are several different medications available that can be used to treat food cravings in order to lose weight. Gastric bypasses are also common and effective. They bypass most of the stomach so that the individual will feel full much faster and not physically be capable of eating any more.
Regulations?
Since it seems like the cause of this obesity problem all comes back to the ingredients in the food we are eating, shouldn’t there be more restrictions and regulations on what companies are allowed to put in processed foods? Other countries have more restrictions on certain food preservatives and contents that they are allowed to include, and overall this seems to be an intelligent, logical idea. Until any laws are passed, however; all that we can do to steer clear of Type 2 diabetes and obesity is to eat whole, nutritious foods and get plenty of exercise. Food companies can tempt us all they want with the high-fat, high-sugar foods they process, but we must look out for our health and do the best we can to resist these foods that will give us brain disease.
For more information related to insulin signaling, energy homeostasis, and glucose metabolism, please visit:
https://moodle.cord.edu/pluginfile.php/625315/mod_resource/content/0/2013%20CNS%20insulin.pdf
The Disease: Obesity
Throughout our media, we see headlines about obesity and the plague-like effect it has over our country. Shows and lifestyle programs are dedicated to stopping obesity. Michele Obama advocated for the elimination of obesity in schools. Messages infiltrate our TVs and radios that tell us to eat less processed food and exercise daily to combat obesity. However, is it possible to avoid or eliminate obesity by simply changing our diet and lifestyle? Or is there more to the problem… Is obesity an actual disease that must be treated with more finesse?
Obesity is indeed an actual disease and despite contrary belief, is not based on laziness or lack of self-control.
In a normal functioning brain, when we consume food, insulin and leptin proteins activate a very specific pathway that leads to ion efflux from specialized brain cells called neurons. This ion efflux of potassium leads to an action called hyperpolarization. Hyperpolarization is important because it slows the neuron firing that tells us to eat more. There are two types of neurons that control our eating: POMC-neurons, which tell us to stop eating, and AgRP-neurons, which tell us to eat more. Insulin acts on these neurons by decreasing the number of AgRP-neurons in the brain and increasing POMC-neurons. Therefore, when we eat and our body releases insulin, we respond by stopping our eating. However, in people who suffer from obesity, overnutrition occurs and normal cellular function becomes cellular stress. Specifically, ER stress leads to physical inflammation of the brain and this inflammation creates insulin resistance. Therefore, the insulin in the brain of someone suffering from obesity does not function properly and cannot tell the body to stop obtaining food. Overall, the effect of overnutrition and obesity becomes a deadly cycle of continual eating and weight gain.
The biological cycle of obesity occurring in the brain cannot be fixed by exercise or dietary changes alone. Drugs that can block the pathway or stimulate normal pathways are more likely to create brain reversals that have a positive effect.
So, the next time we see a show or program about obesity and we are quick to judge the lack of self-control, let us remember that obesity is a disease that physically effects the brain and requires medication or surgery in most cases. It is not a matter of laziness, but of better treatment options and open-mindedness.
http://www.cell.com/trends/endocrinology-metabolism/pdf/S1043-2760(12)00204-4.pdf
Too Much Fat in Your Diet?
From being too busy to simply being lazy, it is really easy to decide against cooking breakfast, lunch, or dinner and going out to eat instead. With McDonalds and Taco Bell being on every street corner, they are easier accessible and family cheap, this makes it way more tempting to eat out than to cook a nice healthy meal at home. On occasion this is perfectly fine, however overtime this can add up and cause all sorts of problems within the body. In today’s society, there is stress beyond belief coming from work, school, family, and friends, which pushes people to eat those unhealthy meals as well. These high fat foods make the body feel temporarily satisfied, which is rewarding and will condition people to continue to eat these foods.

So What is Happening in Your Body?
After having a high fat diet for a prolonged period of time, even after just 72 hours, the body starts to experience something called hyperinsulinemia. This is when there is an excess amount of insulin floating throughout the blood stream. This leads to stress within the brain, more specifically within the endoplasmic reticulum. Due to this ER stress, a couple of different pathways called Socs3 and JNK are activated which, in the end, leads to insulin resistance. Insulin resistance is when insulin produced within the body functions improperly and does not break down glucose. Since glucose is no longer being broken down as frequently as it should, this leads to high blood sugar levels which is a sign of type two diabetes. This process does not happen overnight, and can take years and years of a high fat diet for glucose levels to reach levels of being diabetic. So if you are worried about this happening, chances are its not too late to turn your diet around and reverse these changes.

Type Two Diabetes
Type two diabetes is diagnosed through a series of blood tests. These blood tests simply look at the levels of glucose within the blood and once it reaches a certain point a diagnosis of pre-diabetic or diabetic will be placed on the individual. Some of the symptoms of type two diabetes are increased thirst and urination, increased hunger, numbness or tingling in hands and feet, unexplained weight loss, and having sores that don’t heal properly. The main causes of type two diabetes are being overweight and obese, insulin resistance, the absence of physical activity, and genes. Since this is a genetic form of diabetes, it is possible to be diagnose with it, without being overweight or obese.
Sources:
https://moodle.cord.edu/pluginfile.php/625315/mod_resource/content/0/2013%20CNS%20insulin.pdf
The Science Behind Lou Gehrig’s Disease
Amyotrophic Lateral Sclerosis (ALS) is more commonly known as Lou Gehrig’s disease after the New York Yankee baseball player Lou Gehrig. During his season in 1938, Lou Gehrig started to experience muscle weakness which started to affect his batting and even his ability to tie his shoes. A diagnosis of ALS was soon made, bringing this otherwise not well known disease into the public’s eye.
ALS is characterized by muscle weakness or cramps, cognitive impairments, slurred speech, or difficulty swallowing. The disease often appears with similar symptoms to those of Parkinson’s disease or even Alzheimer’s disease, making the diagnosis of this disease based mainly on ruling out other diseases.
ALS is a degenerative disease that causes death in motor neurons of the brain, spinal cord, and nerves running to muscles. Motor neurons signal movement to occur in muscles by sending a signal from the brain to peripheral muscles. Death to neurons is caused genetics and oxidative stress on the cell.
One of the most important ideas to understanding the science behind ALS is to understand the role of the mitochondria in the cell. The mitochondria are the powerhouse of the cell. It helps to break down molecules so that the cell can use them for energy.
When the mitochondria become overworked, this leads to mitochondrial stress. During mitochondrial stress, extra molecules called oxidants are produced that are harmful to the cell. In response to excessive amounts of oxidants, the cell turns on pathways that signal the cell to die.

Oxidants are the cause of motor neuron death.
There are a few ways to get rid of oxidants. The way that the body normally uses is the SOD1 protein which breaks down oxidants into less harmful substances. Another way is by activation of the OXR1 gene which is the bodies natural response to oxidants. The last way to get rid of oxidants is through antioxidants which protect the mitochondria against oxidative stress.
All of these methods of getting rid of oxidants are currently being used in research to try to slow down the progression of ALS. There are currently no existing treatments for ALS that target oxidants as it can be very hard to target the exact motor neurons where the extra oxidants are forming. Future research will continue to look into oxidants as well as stem cells, optogenetics, and other medications.
Although Lou Gehrig might have been one of the first public cases of ALS, there have been many more cases and much more research conducted since his death. Lou Gehrig died from ALS, but his advocacy for the disease has lead to increased amounts of research, and promise for more effective treatment around ALS.
Information from this post can be found here
To find out more about ALS click here
More information about Lou Gehrig can be found here
Picture is original art work by the author
Obesity – More Than Self-Control?
Obesity is sometimes viewed as a lack of discipline. The obvious fix is start eating healthier and work out a few times a week. Although eating right and exercising are very important, obesity is more than just a weight problem.
There are neurological components to this disease that is plaguing the United States. One component of this very complex illness is the dysregulations of signals being sent in one’s brain.
In the hypothalamus and brain stem, there are specialized neurons called proopiomelanocortin neurons or POMC neurons for short. These neurons are vital players in the story of food control. POMC neurons send projections throughout the brain that let you know you’re full and should stop eating. The POMC works in tandem with a peptide called the agouti-related peptide (AgRP). This peptide is responsible for the signal to eat.
One regulator of POMC is a hormone called leptin. Leptin flows through the blood and when it reaches the brain it binds to the POMC neurons, therefore sending a signal to stop eating. When this process is interrupted in rats, obesity is seen as a result. Other mutations to POMC can lead to adrenal failure, along with early on-set obesity. Therefore, it is evident that this process is vital for maintaining a healthy weight.
This result of over-eating can further damage the body by leading to insulin-resistance. When over nutrition occurs, it can lead to ER stress which activates a pathway called the JNK pathway. This pathway is an inflammatory pathway which ultimately ends in inhibiting the insulin receptor substrates. This inhibition therefore leads to insulin resistance as the insulin signal will no longer be able to be passed on down it’s cascade of signals.
Obesity is large problem in our country. This problem comes with a stigma that those individuals who are obese are weak and have control problems. However, when further examining the components of this disease there are many neurological components. It is an imbalance of chemicals and other peptides. Therefore, I believe that with more research obesity will shift to being seen as a brain disease as well, hopefully improving the treatment and reducing the incidence.
For more reading on obesity and the brain, please check out:
http://www.cell.com/trends/endocrinology-metabolism/fulltext/S1043-2760(12)00204-4
ALS and Oxidative Stress – A Possible Culprit
ALS is a complicated and sinister illness. Over time it deteriorates the motor neurons in your brain and spinal cord, trapping its victims inside of their own bodies. Researchers are looking into how oxidative stress plays a role into causing this heartbreaking disease.
Oxidative stress is a result of the mitochondria, the organelle that makes energy in the cell, not being able to keep up with detoxifying the hazardous reactive products of oxygen. An increase in oxidative stress is considered to play a large role in the development of ALS.
When oxidative stress occurs it causes proteins to gather in the cytoplasm, which is where they are not suppose to be. This new aggregation of proteins combines with naturally occurring stress granules. For short periods of times, stress granules are beneficial. However, when present for long periods of time the beneficial effects turn into hazardous effects.
These harmful bundles in the cytoplasm can lead to misfolded proteins. The body has it’s own safety guard to protect against misfolded proteins. This safety guard is called the unfolded protein response (UPS).
https://www.nature.com/articles/nm0410-396
The unfolded protein response is the cell’s response to proteins that are made incorrectly. This response monitors the amount of proteins that are defective and when the number of defective proteins are too high it halts the production of proteins. This stop in protein making is done in order to correct the current mistakes. However, if this process takes to long the goal of the UPS switches form restoration to destruction causing the cells to initiate apoptosis, or cell death.
Therefore, increased and decreased amounts of UPS have been seen in ALS patients. With a low UPS there are many unfolded and misfolded proteins in the body not behaving as they should be, and with the upregulation of UPS many cells are dying.
Oxidative stress seems to be one of the culprits for initiating this cascade of negative effects and should continue to the a main point of focus in future research. With more research and understanding, hopefully one day a more curative treatment will be developed.
For more reading on the topic, please check out:
https://www.ncbi.nlm.nih.gov/pubmed/27150074