 pexels.com stock photo by Darya Sannikova
pexels.com stock photo by Darya Sannikova
Antisocial personality disorder (ASPD) is a mental health condition characterized by disregard for the rights of others, impulsivity, and a lack of empathy. Environmental factors such as childhood experiences, parenting style, and social influences can contribute to the development of ASPD. Childhood abuse, neglect, and inconsistent discipline can increase the risk of developing ASPD. Parental antisocial behavior, substance abuse, and criminal behavior can also contribute to the development of the disorder. Additionally, exposure to peer pressure, deviant behavior, and criminal activities can increase the likelihood of developing ASPD. Environmental factors can interact with genetic predispositions to shape the development of the disorder, highlighting the importance of early intervention and prevention efforts [4].
Genetics
Antisocial personality disorder (ASPD) has been found to have a strong genetic component, with heritability estimates ranging from 40% to 70%. The LINC00951 gene has recently been identified as a potential genetic risk factor for antisocial personality disorder (ASPD). Research has found that individuals with ASPD have decreased expression of LINC00951 in the prefrontal cortex compared to those without the disorder. This gene is involved in the regulation of neuronal gene expression and plays a role in the development of the prefrontal cortex, a brain region implicated in the pathology of ASPD. Decreased expression of LINC00951 may contribute to impaired prefrontal cortical function, which is associated with the impulsivity and disregard for others’ rights characteristic of ASPD. Further research is needed to fully understand the role of LINC00951 in the development of ASPD [3].
ASPD and the Brain
Recent advances in neuroscience have shed light on the neural correlates of antisocial personality disorder (ASPD). Studies have found differences in brain structure and function between individuals with and without ASPD. For example, reduced gray matter volume in the prefrontal cortex, amygdala, and hippocampus have been observed in individuals with ASPD. Functional imaging studies have also revealed abnormalities in brain regions involved in emotion processing, decision making, and empathy. These findings suggest that ASPD may be associated with dysfunction in neural circuits involved in social and emotional processing. Further research in this area may help to inform the development of more effective treatments for ASPD.
History and Current Terminology
Antisocial personality disorder (ASPD) has a long history of various names and classifications. Early descriptions of the disorder can be traced back to the 1800s, when it was referred to as moral insanity. The term sociopathy was later introduced in the early 1900s, followed by psychopathy in the mid-20th century (Figure 1). In the 1980s, the Diagnostic and Statistical Manual of Mental Disorders (DSM) introduced the term antisocial personality disorder, which is still in use today. The current DSM-5 criteria for ASPD include a persistent pattern of disregard for the rights of others, impulsivity, and a lack of remorse or guilt. Despite changes in terminology and classifications, the core features of the disorder remain consistent [2].
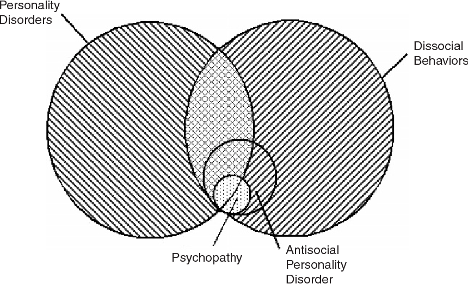
Figure 1. Antisocial behavior disorder and other mental health disorders
ASPD Subtypes
Antisocial personality disorder (ASPD) can be classified into two subtypes: primary and secondary. Primary ASPD is characterized by fearless dominance, manipulativeness, and a lack of anxiety. These individuals may display charisma and leadership skills, but their behavior is often harmful to others. Secondary ASPD is characterized by impulsivity, aggressiveness, and a lack of remorse or guilt. These individuals may engage in criminal behavior, substance abuse, and risky behaviors. The distinction between these subtypes can be useful in understanding the different underlying mechanisms and treatment approaches for ASPD. However, the diagnosis of ASPD is often based on the presence of a set of specific criteria, rather than subtype classifications.
Treatments
Antisocial personality disorder (ASPD) is a challenging condition to treat, as individuals with the disorder often lack motivation to change their behavior and may not perceive their behavior as problematic. However, there are several treatments that have been shown to be effective in reducing symptoms of ASPD. Cognitive-behavioral therapy (CBT) can help individuals with ASPD learn new coping skills, identify and change negative thought patterns, and improve interpersonal functioning (Figure 2). Medications such as mood stabilizers and antidepressants may also be useful in managing conditions such as depression or anxiety [1].

Figure 2. Drug treatment and talk therapy may be helpful for antisocial personality disorder, however this condition is very challenging to treat.
Resources
[1] Haelle, T. (2022, October). How to treat antisocial personality disorder. EverydayHealth.com. Retrieved April 5, 2023, from https://www.everydayhealth.com/antisocial-personality-disorder/treatment/
[2] Kiehl, K. A., & Hoffman, M. B. (2011). The criminal psychopath: History, neuroscience, treatment, and economics. Jurimetrics. Retrieved April 5, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4059069/
[3] Tiihonen, J., Koskuvi, M., Lähteenvuo, M., Virtanen, P. L., Ojansuu, I., Vaurio, O., Gao, Y., Hyötyläinen, I., Puttonen, K. A., Repo-Tiihonen, E., Paunio, T., Rautiainen, M.-R., Tyni, S., Koistinaho, J., & Lehtonen, Š. (2019). Neurobiological roots of psychopathy. Molecular Psychiatry, 25(12), 3432–3441. https://doi.org/10.1038/s41380-019-0488-z
[4] Tuvblad, C., & Beaver, K. M. (2013, September). Genetic and environmental influences on antisocial behavior. Journal of criminal justice. Retrieved April 5, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3920596/