What is a mild traumatic brain injury and how do they happen?
Mild traumatic brain injuries (TBIs) are also referred to as concussions. They occur due to not only a bump or blow to the head, but also jolting the head too quickly. Essentially, the hit and movement of the head moves the brain too quickly. This causes chemical changes and stretching and damaging to brain cells. These are very serious injuries that may result in various symptoms [1]. Common symptoms of a concussion often mirror that of migraines including headaches, dizziness, nausea, and more. However, depending on the extent of the injury, it may result in cognitive and behavioral alterations [2].
What events take place in the brain after a mild TBI?
An article by Giza and Hovda discusses the fundamental neurometabolic cascade post-concussion (2014). The authors explain that the injury first begins with a potassium efflux, meaning it is leaving the cell, and sodium and calcium influx where these molecules flood into the cell. This triggers channels (voltage and ligand gated) to open and defuse through the rest of the cell. In an attempt to return to homeostasis, ATP membrane ionic pumps begin to work harder, and intracellular calcium is released, which furthers the energy crisis occurring in the cell because ATP is being utilized too much alongside mitochondrial dysfunction.
More specifically, intra-axonal calcium that is released to return the cell to homeostasis causes damage to neurofilaments and microtubules. This causes axonal dysfunction or even disconnection as these are two structures that are critical for structure and transportation within the axon. Each of these occurrences within the cell change ligand-gated excitatory and inhibitory neurotransmission, specifically for glutamate and GABA. Ultimately, downstream signaling and influx development is impacted causing vulnerability to comorbidities like anxiety disorders [2].
Common comorbidities
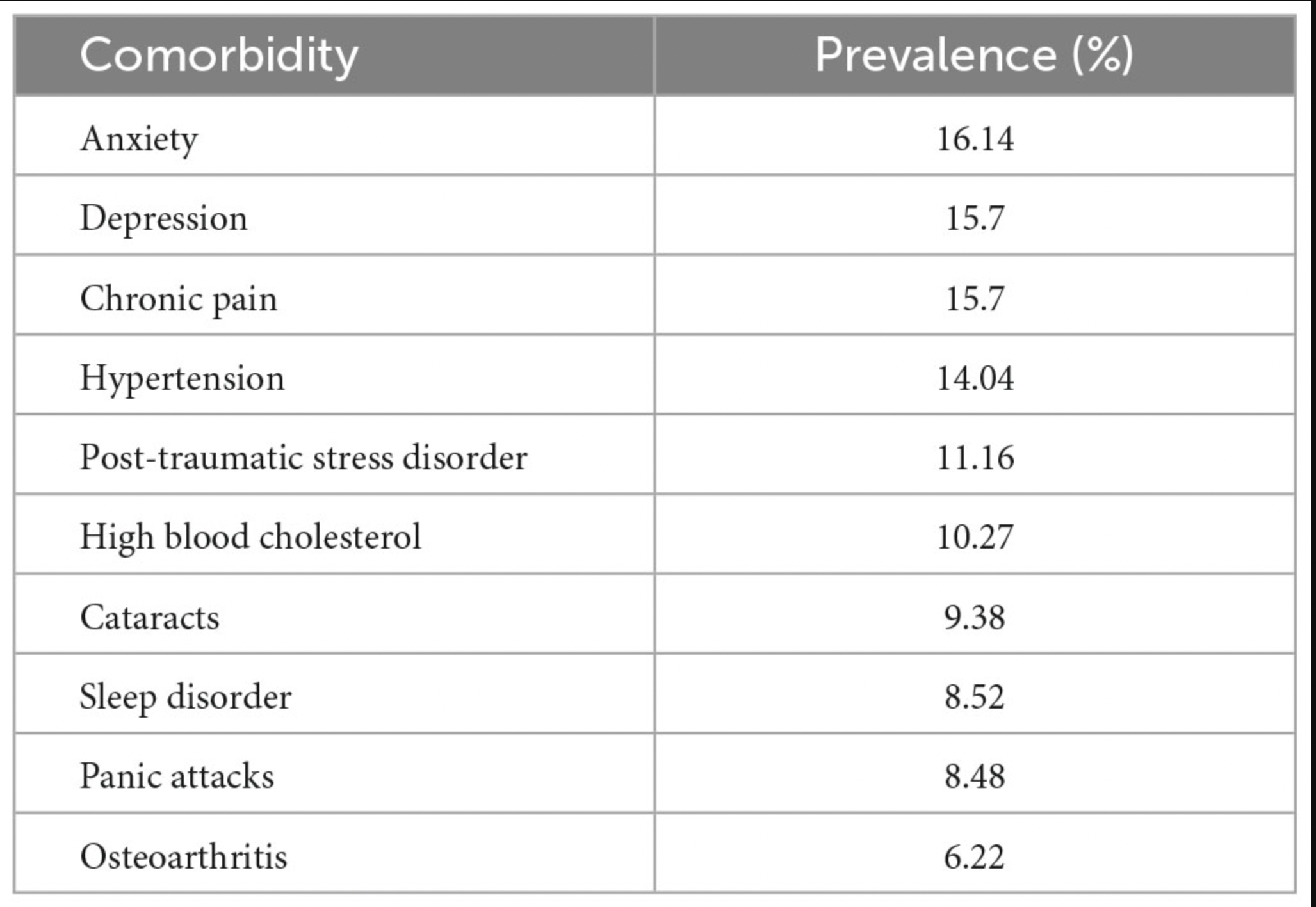
While neurological and psychiatric comorbidities are most commonly thought of due to the bodily region of the injury, others such as cardiovascular, endocrine, and respiratory can commonly occur as well. This makes sense because the brain is the control center for the rest of the body. Excitatory and inhibitory neurotransmission not only tells your body how to feel but also how to act. However, psychiatric comorbidities are among the most prevalent. Figure 1 displays the top 10 comorbidities seen in individuals as stated from a study by Sudhakar et al. (2023). The authors of this study explain how comorbidities are most likely to occur five years after the TBI has occurred with younger individuals (<50 years of age) being at increased risk for them [3].
Figure 1. Top 10 comorbidities with concussions [3].
Long term comorbidities and disorders
After repeated exposure to TBIs or more severe head injuries, long term neurological disorders may occur due to permanent damage in the brain such as cell death. Examples of these may include Chronic Traumatic Encephalopathy (CTE) which occurs after repeated head injuries which lead to a buildup of tau proteins, causing cognitive and behavioral changes. Another is Post-Concussion Syndrome (PCS) where the symptoms of the concussion last for an extended period of time. Interestingly, because of the connection of tau proteins, plaques, and cell death, risk for neurodegenerative diseases is also possible as the accumulation of brain damage may contribute to diseases such as Alzheimer’s. However, this proposition has yet to be studied further [4].
Tying it all together
Overall, mild TBIs are serious injuries that must be taken seriously. The neurometabolic cascade that occurs after them pose irregularities in excitatory and inhibitory neurotransmission that may contribute to different forms of comorbidities depending on where the brain is injured. This, as shown in figure 2, all comes together as the overall concussion symptoms that the individual faces. These comorbidities consist of psychiatric disorders such as depression and anxiety, cardiovascular comorbidities like hypertension, musculoskeletal, and more. Furthermore, even after the individual returns to normal activities, comorbidities may occur both short term and long term.
Figure 2. Conditions leading to overall concussion symptoms.
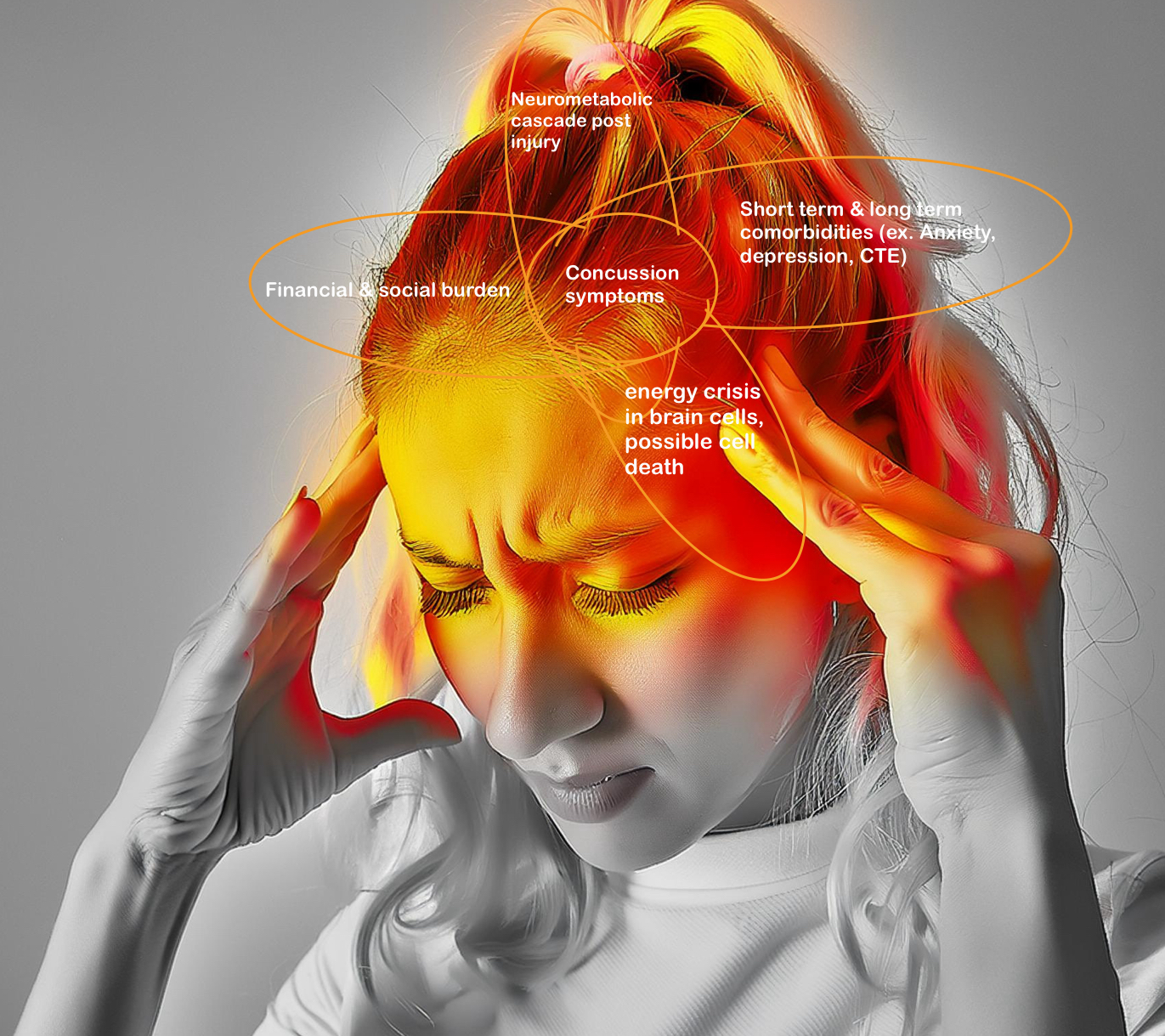
Fig.2. artstract created by M. Olson
Resources
[1] Mild TBI and Concussion | Concussion | Traumatic Brain Injury | CDC Injury Center. (2022, November 14). https://www.cdc.gov/traumaticbraininjury/concussion/index.html
[2] Giza, C. C., & Hovda, D. A. (2014). The New Neurometabolic Cascade of Concussion. Neurosurgery, 75(0 4), S24–S33. https://doi.org/10.1227/NEU.0000000000000505
[3] Sudhakar, S. K., Sridhar, S., Char, S., Pandya, K., & Mehta, K. (2023). Prevalence of comorbidities post mild traumatic brain injuries: A traumatic brain injury model systems study. Frontiers in Human Neuroscience, 17. https://doi.org/10.3389/fnhum.2023.1158483
[4] Madwire. (2023, September 21). Understanding the Link Between Concussions and Neurological Disorders. Atlanta Neuroscience Institute. https://atlneuroinstitute.org/blog/understanding-the-link-between-concussions-and-neurological-disorders/
