Metabolic syndrome and obesity have become pressing health concerns worldwide, affecting millions of individuals across all age groups. Even Though these conditions are interpreted to be more like personal health matters, their impact extends far beyond individual lives. Metabolic syndrome and obesity pose significant challenges to public health systems, communities and individual lives. Therefore, understanding and addressing these issues is crucial for everyone.
What should the public know about metabolic syndrome and obesity?
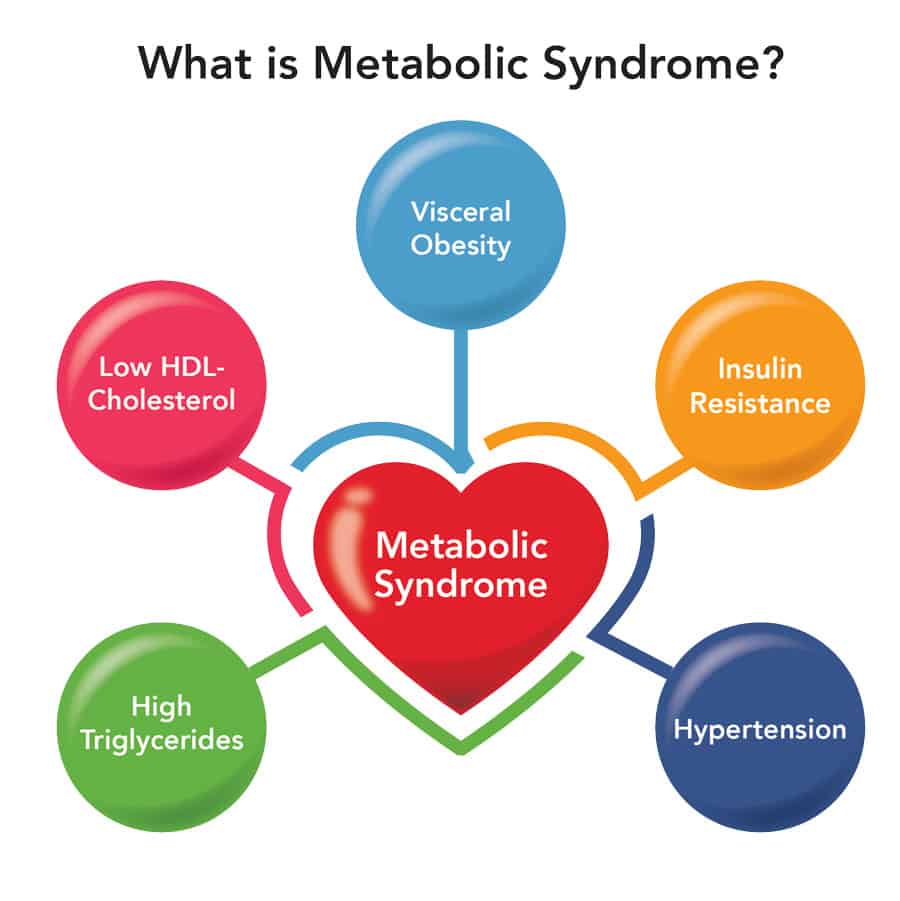
Firstly, these conditions are closely linked to a multitude of serious health problems. High blood pressure, elevated blood sugar levels, abnormal cholesterol levels, and excess abdominal fat are all risk factors associated with Metabolic syndrome[1]. These factors can significantly increase the risk of developing other chronic diseases such as type 2 diabetes, heart disease and even certain types of cancer[2]. Obesity, often a component of metabolic syndrome, can further worsen these risks, leading to a higher likelihood of premature death and decreased quality of life.
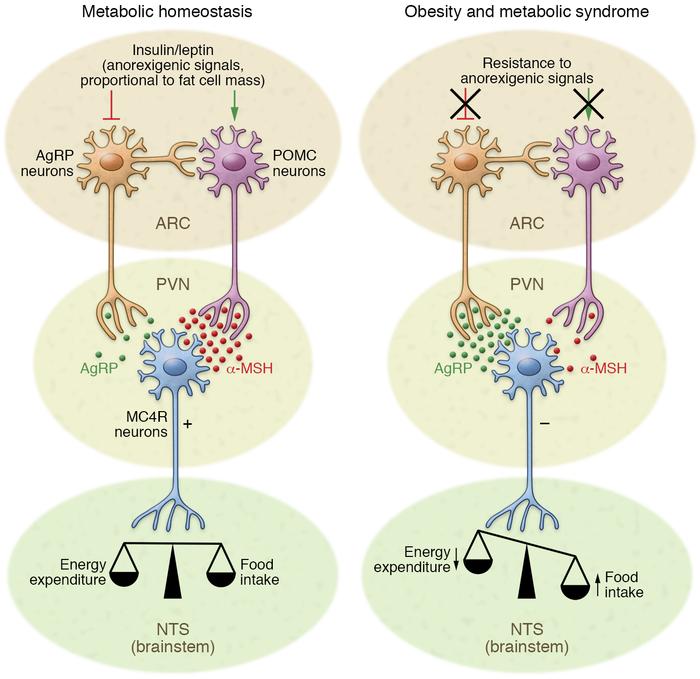
In the article “Hypothalamic inflammation in obesity and metabolic disease”, by Alexander Jais and Jens C. Brüning, they discuss the role and relationship that hypothalamic inflammation has to do with metabolic disease and obesity. The authors discuss how chronic overnutrition, characterized by excessive intake of high-calorie, high-fat diets, triggers a state of low-grade inflammation in the hypothalamus[3]. This inflammatory response involves the activation of resident immune cells such as microglia and the infiltration of peripheral immune cells into the brain. These immune cells release pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β), which disrupt normal hypothalamic neuronal function, and instigate inflammation in the hypothalamus[3].
One critical consequence of hypothalamic inflammation is the development of leptin and insulin resistance. Leptin and insulin are key hormones that signal satiety and regulate energy balance. However, in the context of obesity and hypothalamic inflammation, the responsiveness of hypothalamic neurons to these hormones is impaired, leading to a failure to suppress appetite and promote energy expenditure effectively[3].
Why should the public care about metabolic syndrome and obesity?
Beyond individual health, the implications that metabolic syndrome and obesity have on society and the economy are extensive. The burden on healthcare systems is immense, with billions of dollars spent annually on medical treatments, medications, and interventions related to these conditions[4]. Additionally, metabolic syndrome and obesity disproportionately affect marginalized communities and contribute to health disparities. Factors such as socioeconomic status and access to healthcare play significant roles in the prevalence and management of these conditions. Addressing these disparities requires collective action and societal awareness[5].
Despite these challenges, there is hope in ongoing research and interventions aimed at combating metabolic syndrome and obesity. Scientists are continually uncovering new insights into the complex biological mechanisms underlying these conditions. From understanding the role of genetics and hormones, to exploring the influence of gut microbiota and environmental factors, research is helping us to develop innovative prevention and treatment strategies[6].
It’s important for the public to recognize that metabolic syndrome and obesity are not simply personal issues but rather societal challenges that require collective action. Whether it’s making healthier food choices, engaging in regular physical activity, or supporting policies that prioritize public health, everyone has a role to play in tackling these issues.

References
Jais, A., & Brüning, J. C. (2017). Hypothalamic inflammation in obesity and metabolic disease. The Journal of Clinical Investigation, 127(1), 24-32.
National Heart, Lung, and Blood Institute. (n.d.). Metabolic syndrome. Retrieved from https://www.nhlbi.nih.gov/health-topics/metabolic-syndrome
World Health Organization. (2021). Obesity and overweight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Centers for Disease Control and Prevention. (2021). Adult obesity facts. Retrieved from https://www.cdc.gov/obesity/data/adult.html
World Health Organization. (2016). Obesity and overweight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
United States Department of Agriculture. (n.d.). Economic costs of obesity. Retrieved from https://www.ers.usda.gov/webdocs/publications/94849/err270_summary.pdf?v=9633.4
Reilly, J. J., & Kelly, J. (2011). Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. International Journal of Obesity, 35(7), 891-898.
Gloy, V. L., Briel, M., Bhatt, D. L., Kashyap, S. R., Schauer, P. R., Mingrone, G., & Bucher, H. C. (2013). Bariatric surgery versus non-surgical treatment for obesity: A systematic review and meta-analysis of randomised controlled trials. BMJ, 347, f5934.