Picture 1: Impact to the brain[1].
Concussion or mild traumatic brain injury(mTBI) is something that is prevalent, especially within sports, and something quite a lot of people experience in their lifetime. Recently, there has been an increase in the interest in researching the biological bases of concussions, and with more advanced neuroimaging it allows to look at the pathophysiology post-injury.
Definition of concussion/mild TBI:
The hallmarks of concussion or mTBI can be defined by having impaired neurobiological signs and symptoms after having biomechanical force to the brain. Described as a neurometabolic cascade of events, these involve bioenergetic challenges, cytoskeletal and axonal alterations, impairments in neurotransmission, vulnerability to delayed cell death and chronic dysfunction. It was found in adult animals that the impaired metabollism that comes post-injury can last up from 7 to 10 days, and was additionally found to be associated with behavioral impairments in spatial learning[2].
Symptoms and signs of concussion: [3]
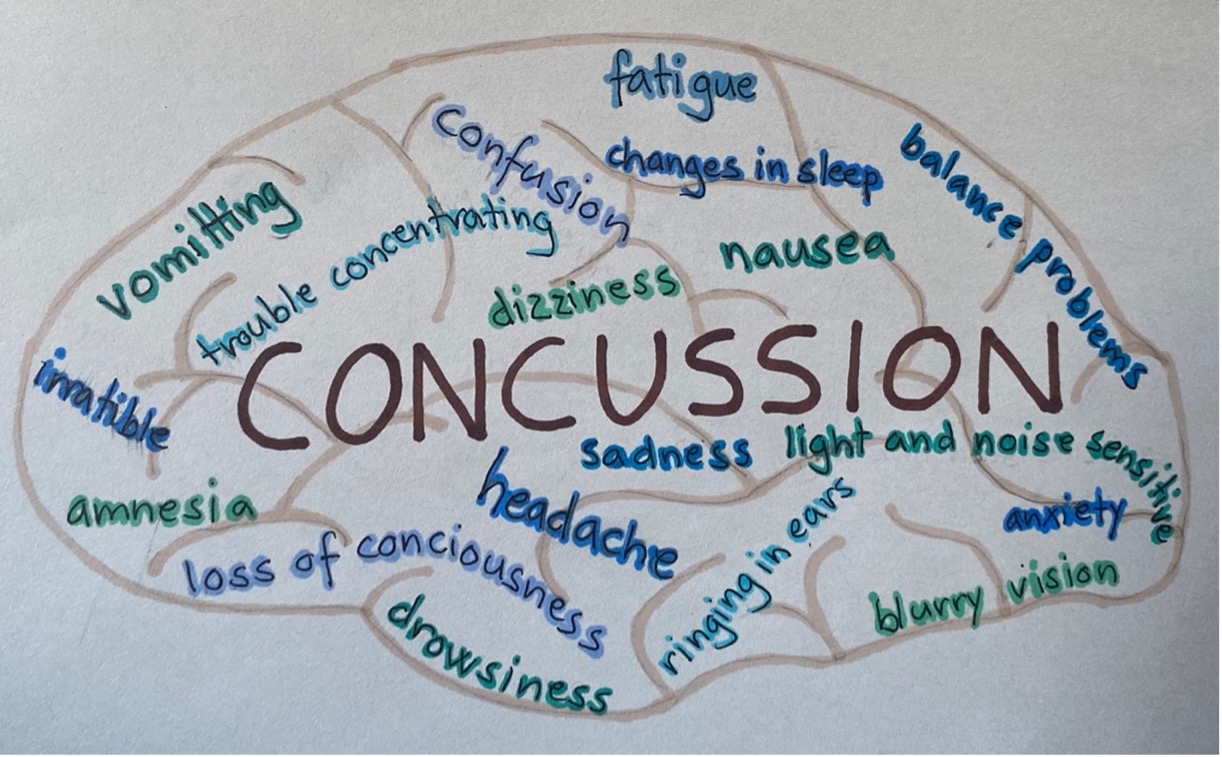 Artstract: Typical symptoms and signs of concussions illustrated.
Artstract: Typical symptoms and signs of concussions illustrated.
The acute pathophysiology:
There are a various acute neurometabolic changes that occur in the brain after a concussion and has been described as a neurometabolic cascade of events. This cascade involves bioenergetic challenges, axonal and cytoskeletal alternations, neurotransmission impairments, vulnerability to delayed cell death and chronic dysfunction[4].
As illustrated in Figure 1 an ionic flux and hyper acute indiscriminate glutamate release happens as a result of the biochemical injury. In an effort to restore the ionic and homeostasis, the membrane ionic pumps that are APR causing hyperglycolysis (overdrive). This created relative depilation of intracellular energy reserves, and also increases levels of ADP. The intra-axonal calcium flux can result in loss of structural integrity in axons and cause cytoskeletal damage as neurofilaments side-arms can be phosphorylated and collapse. Further the damages to the neurofilaments and additionally microtubules lead to axonal dysfunction and is potential for disconnection. Lastly, an alteration in glutamate, NMDA, receptor subunit composition and function can be found after a concussion, this alters neurotransmission. This alteration interferes with normal developmental plasticity, electrophysiology, and memory[5].
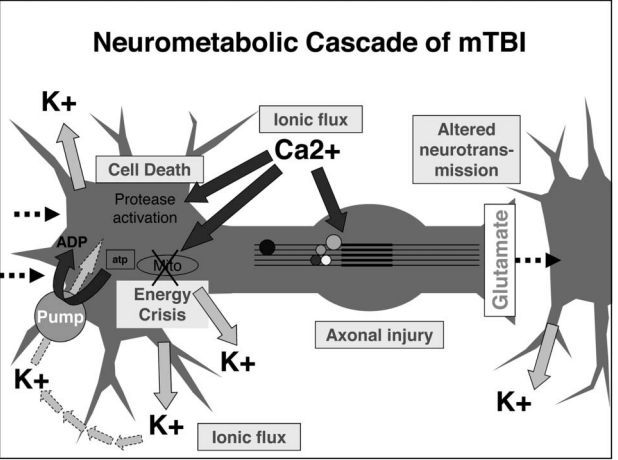
Figure 1: The acute cellular biological processes that occur after a concussion or a mTBI[6].
The various activations and infiltrations of the microglia was found to cause inflammatory changes in the brain. After a TBI there is an extensive upregulation of cytokine and inflammatory genes. While for cell death, mTBI generally show little cell death, but with the impact of repeated mTBI may cause functional impairments, and there may be longer-term structural changes[7].
As for the repeated concussive injuries since the intracellular redox state is altered in the concussed brain if it`s hit with another impact it puts additional stress on the damaged free radicals and shifted metabolic pathways. That can trigger impairments that are longer lasting and is why the brain is more vulnerable to repeated injury[8].
Age differences with susceptibility and severity:
The young brain concusses more easily than the adult brain and can often have worse prognosis for the outcomes after the injury[9]. mTBI has demonstrated damage to white matter and have been associated with cognitive impairments. The injury disturbs growth and development in the brain. It was found in 2017, that TBI is the leading cause of death and disability in children[10]. As for adults over the age of 65, they were found to be four times more likely to have a negative outcome from a mTBI[11]. Additionally, there might be a gender difference in susceptibility for concussion, where females are more susceptible than males.
BIBLIOGRAPHY
[1] What to do if someone is showing concussion symptoms. (2022, July 25). Livi. https://www.livi.co.uk/your-health/concussion-symptoms/
[2] Giza, C. C., & Hovda, D. A. (2014). The new neurometabolic cascade of concussion. Neurosurgery, 75 Suppl 4(0 4), S24–S33. https://doi.org/10.1227/NEU.0000000000000505
[3] Concussion; Symptoms and causes. Mayo Clinic. (2024, January 12). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594
[4] Giza, C. C., & Hovda, D. A. (2014). The new neurometabolic cascade of concussion. Neurosurgery, 75 Suppl 4(0 4), S24–S33. https://doi.org/10.1227/NEU.0000000000000505
[5] Ibid.
[6] Ibid.
[7] Ibid.
[8] Ibid.
[9] Tator C. H. (2013). Concussions and their consequences: current diagnosis, management and prevention. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 185(11), 975–979. https://doi.org/10.1503/cmaj.120039
[10] Araki, T., Yokota, H., & Morita, A. (2017). Pediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and Management. Neurologia medico-chirurgica, 57(2), 82–93. https://doi.org/10.2176/nmc.ra.2016-0191
[11] Lele A. V. (2022). Traumatic Brain Injury in Different Age Groups. Journal of clinical medicine, 11(22), 6739. https://doi.org/10.3390/jcm11226739
