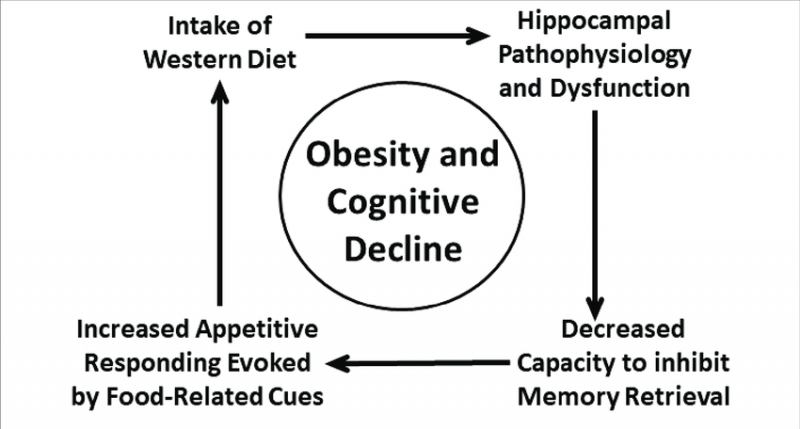
Obesity and cognitive decline; how closely related could they be really? As it turns out, the connection between these two can be mediated by one step. Insulin Resistance. A high fat diet leads to an increase in meta-inflammation, and if this inflammation becomes chronic, we see the development of Insulin Resistance, then ultimately Type 2 Diabetes. Now certainly obesity and diabetes are no small factors in one’s life. But what if I told you that’s not where it stops? The insulin resistance caused from a fatty diet and/or obesity, is also believed to be a major underlying cause of Alzheimer’s disease. Researchers have shown that obesity nearly doubles the risk of Alzheimer’s disease in later life, and even if remaining healthy, obesity has been related to an increase in risk of Mild Cognitive Impairment, regardless of age. These findings have also been recreated in animal models. 
Now when you think of insulin, I’m sure most people will think of the same things, diabetes, blood sugar, released by the pancreas. Now take a look at this figure.
At a cellular level, insulin does so much more than just that! Even outside of AD specifically, researchers have shown that those with an increased BMI, and type 2 diabetes, had more atrophy in the frontal, temporal, and subcortical parts of the brain, which are all typically associated with learning and memory. The reasoning behind the obesity/insulin resistance connection, is that obesity and it’s increase in adipose tissue results in a low level metabolic inflammation. This inflammation releases cytokines, and by looking at the figure below, you will see that the products of these inflammatory cytokines binding, actually inhibits the actions of insulin and insulin binding.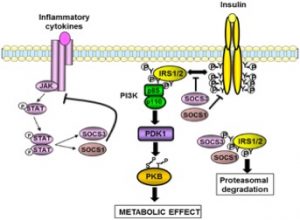
Finally, moving into Alzheimer’s and Dementia. Studies have shown that elderly people with morbid obesity had a higher level of hippocampal markers that are associated with β-amyloid
Plaques, as well as tau protein accumulations, along with a decreased hippocampal volume. The hippocampus is important in the formation of long-term memories, and between the appearance of plaques, and neurofibrillary tau tangles, along with a decrease in the hippocampus itself, we see the building blocks of AD. For so long, when looking at obesity it was always “heart health” and that was the major focus, I think it now may be important to reference the risks associated with the mental well-being of individuals as well. On the flip-side, It should be noted that not all obesity’s are made the same. The major difference is metabolically healthy, vs unhealthy. Metabolically unhealthy, means insulin pathways have already been damaged, and changed (i.e. Type 2 Diabetes). This can be treated, but ultimately not cured. Metabolically healthy means that although the diet has increased inflammation, and begun to exhibit somewhat insulin resistant effects, it is not ‘chronic’, and the insulin pathway is still ‘rescuable’. That means that although it is problematic, if a proper diet, is instituted, and the person can get back to a healthy body composition, the long-lasting effects of this inflammation will be less serious, and they would no longer be within the realms of major obesity related risk factors. As we learn more about the interrelation of these conditions, it is important to recognize the longer-reaching issues that they may present down the road. I believe the more people know about the dangers they are presenting to their bodies, the better the chance they will take the necessary steps to maintain their bodies adequately.