Marijuana has been a heavy topic in the last few years. Twenty nine states have passed laws either legalizing medical marijuana or for recreational use. Changes are occurring in our country regarding marijuana, so should our education about it also change?
When I was in high school, I had the typical health class that lasted about two months during my freshman year. We grazed over topics that included drugs, mostly focusing on the “harder” drugs which have more adverse and visible effects on the user. We were shown pictures, which were intended to make us scared about using the drugs. We also talked about alcohol quite a bit. It was drilled into us how alcohol use is bad and how alcoholism can ruin your life. But, the topic of marijuana wasn’t really touched on.
 With the legalization of the drug in many states, I think that marijuana should be a topic which is focused on in schools. When alcohol was first legalized, nobody really knew how it affected the body. People would drive home after going to a bar and did not necessarily know about its addictive powers. Now, we are well aware of all of the negative side effects and long-term addictive properties of alcohol. Education has always been highly focused on alcohol, but why can’t we be pro-active about our education on marijuana?
With the legalization of the drug in many states, I think that marijuana should be a topic which is focused on in schools. When alcohol was first legalized, nobody really knew how it affected the body. People would drive home after going to a bar and did not necessarily know about its addictive powers. Now, we are well aware of all of the negative side effects and long-term addictive properties of alcohol. Education has always been highly focused on alcohol, but why can’t we be pro-active about our education on marijuana?
We are in the beginning stages for marijuana legalization, just like we were with alcohol. But, I think that schools should devote more time to education their students about marijuana, just like we already do with alcohol. With it becoming more and more integrated in our society, students should know just what it does in order to make good decisions if they come into contact with it. I know that as a country we are still in the beginning phases, so more research does need to be done in order to determine if there are any possible long-term effects. But, for now, we can choose to be pro-active and commit to teaching society about marijuana, so that down the road more people are more informed about the drug.
Concussed? Sit It Out Pal, You’ll Thank Me Later!
Most athletes who play any contact sport at whatever level can relate to the guilt of injury, the feeling of not being there for your brothers and sister to fight for that W, bring that trophy home to a bunch of rabid fans, satisfy your own insatiable competitive will, prove the haters wrong, I get it, I’ve felt that too. To parents who’s offspring have dealt with a sports related injury, perhaps you are worried sick and want them to recover like yesterday so your kid can get off the couch, make some friends, learn to be tenacious, gracious in the face of defeat, disciplined even when it is physically painful, all of which are admirable traits that sport teaches us. To the service member who got concussion while out there training and fighting to ward off enemies both home and abroad, is eager to prove his worth to his fellow troops, eager not to let his family down, eager to please his commander, give me an ear. Today, I write to plead with you all: Concussed? Sit it out pal, you’ll thank me later! A concussion is defined as a clinical syndrome characterized by immediate and transient alteration in brain function, including alteration of mental status and level of consciousness, resulting from mechanical force or trauma. Here is what follows physiologically.
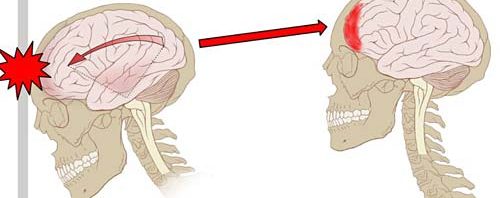
A concussed individual may develop cerebral edema, accounting for loss of consciousness, memory impairment, disorientation and headache. The Brain’s auto regulatory mechanisms compensate for this mechanical and physiologic stress and protect against massive swelling by acutely limiting cerebral blood flow, which leads to accumulation of lactate and intracellular acidosis. A state of altered cerebral metabolism occurs and may last ten days, involving decreased protein synthesis and reduced oxidative capacity. Loss of consciousness after head injuries, the development of secondary brain damage, and the enhanced vulnerability of the brain after an initial insult can be explained largely by characteristic ionic fluxes, acute metabolic changes, and cerebral blood flow alterations that occur immediately after cerebral concussions. Extracellular potassium concentration can increase massively in the brain after concussion, followed by hypermetabolism lasting up to ten days. This makes the brain more vulnerable and susceptible to death after a second sub-lethal insult of even less intensity.
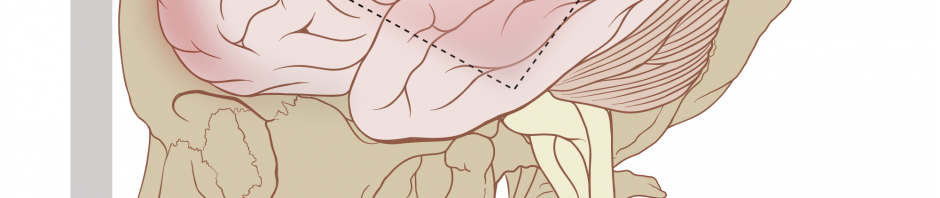
Second Impact Syndrome (SIS), first described by Richard L. Saunders, MD and Robert E. Harbaugh, MD in 1984, consists of two events. Typically, it involves a patient suffering post-concussive symptoms following a head injury. If the patient sustains a second head injury/concussion, diffuse cerebral swelling, brain herniation, and death can occur. Though it is rare, it is devastating in that young, healthy patients may die within a few minutes. Fisher J, and Vaca F, hence conclude that when the patient sustains a “second impact,” the brain loses its ability to auto regulate intracranial and cerebral perfusion pressures. In severe cases, this may lead to cerebral edema followed by brain herniation. In a few implicated cases, death has been reported to occur in a matter of two to five minutes, usually without time to stabilize or transport an athlete from the playing field to the ED. This demise can occur far more rapidly than that of an epidural hematoma. Recent research has pointed out that brain swelling in minor head trauma is more significant in small children than in adults. The term “malignant brain edema” has been used to describe this phenomenon. Though more research in this area is necessary to determine if and when malignant brain edema and SIS are related, or even if they occur by the same process, it is unquestionable that getting back on the field of play or re-engaging in contact activity before a concussion is fully healed makes one more vulnerable to sustaining a second concussion. So again I say and again I plead, sit it out pal, you’ll thank me later!
Concussions: An Invisible Disease
According to the Center for Disease Control, Americans sustain approximately 3.8 million concussions annually from sports and other recreational activities. The risk is particularly high for high school and college athletes who not only have increased exposure for opportunities to sustain a traumatic brain injury (TBI), but their brains are increasingly vulnerable as they are still undergoing development.
The true seriousness of concussions if often either disregarded or goes unnoticed due to the fact the damage is typically on a microscopic rather than macroscopic level. In fact, many individuals that have been concussed show little to no observable or physical changes, unless exposed to specific conditions which result in an overuse or overstimulation of the injured area of the brain.
It is for this reason that concussions are often seen as in invisible disease. They are often disregarded, or warily acknowledged at best, both of which can be detrimental for the recovery of the concussed individual.
Recovery from a concussion should be regarded with utmost importance and is not something to be ignored. Unlike a sprained ankle or broken arm, it is difficult to isolate and prevent use of the brain. To stop thinking is to stop functioning – to stop being a human, to stop living. It simply is not possible. As such, the brain takes longer to heal as it must continue to function all the while. That is not to say it should continue to function at normal (prior concussion) levels. In order for proper and expedited recovery, use of the brain should be limited when possible.
Athletes are often at the highest risk for concussions (particularly college or professional) and stand to experience the most harmful effects (on a yet developing brain) if their injuries are not treated properly. Sadly, they are also met with the most difficult situations when facing a proper and hasty recover.
All too often, a concussed athlete is met with skepticism and doubt, as well as resistance. Sadly, this is often received from their educators. Concussions are an immediate injury and often difficult to comprehend. One day the student is fine, working on homework or taking a test, the next, they may have difficulty coherently reading a paragraph. This drastic change in ability can, understandably, be difficult to accept. However, it is imperative that we do. For the best possible recovery, most physicians suggest that student athletes take a complete break from school, following the injury. This period of time or “break” can vary in duration depending on the individual and the severity of the concussion. Following this “break” the individual typically follows a return to learning protocol, which gradually eases them back into the academic rigor they previously experienced. If the concussed individual is not supported and encouraged to follow these important recovery processes, it may prevent them from healing properly and take them far longer than it should.

Even with support, playing “catch up” after such an academic break can be daunting and perhaps impossible. Understanding that teachers/professors must be fair to all of their students, I think it is a worthy goal to search for methods (either as a professor or as a college) that can allow students who sustain a TBI to remain on track academically without having to drop a class, or be overloaded with material to catch up.
Even more important than academic support, in my opinion, is the support and understanding these concussed athletes receive from their coaches. In many cases, especially because concussions can be undetectable without significant testing, a coach may witness a potential cause for concussion and let it go unreported or unnoticed. They are not alone as many athletes may well choose to disregard the possibility of concussion, whether purposefully or unknowingly. However, in the case of concussions, all precautions should be taken. Second impact syndrome is a very real disease which occurs when a “second impact” or TBI is sustained before the healing process of the first has been completed. This can result in diffuse cerebral swelling, brain herniation, and death.

It is for this reason that a high expectation of responsibility and observation must be placed on coaches. It is difficult to bench the star player in the final minutes of a tie game, even more so if the player doesn’t feel as though they need to sit out. However, it is a coach’s duty to objectively view the situation and do what is in the best interests for the health of their athlete, whether the athlete protests or whether it costs the team the game.
It is important that we rid the stigma that can often come with concussions. Just because it may seem “invisible”, does not mean it should be treated as such, and devastating effects can occur if it is. It is imperative that we determine a method as coaches, teachers, individuals etc. to look objectively at situations involving concussions and work to provide the best care and best environment for an individual to recover and prevent further damage.
New Evidence Shows Immediate Effects of Soccer Headers
As a former soccer player who has suffered three in-game concussions, I’ve often wondered about the effects that “routine” headers have on the brain. When I played as a defender, I sometimes took 15 to 20 headers per game off of goal kicks. Most times, these balls would plummet from high in the sky and if I didn’t hit them just right, I experienced a stinging sensation that occasionally resulted in short headaches. Despite the fact that my concussions were a result of head to head collisions and not common headers, I’ve been more interested in what these sub-concussive and repeated hits to the head can do to the brain. Ultimately, if these routine headers are affecting the brain, steps must be taken to improve player safety.
In October of 2016, a study about cognitive and electrical changes in the brain following routine headers was published in EBioMedicine. Presently, it is undeniable that soccer has detrimental effects of the brain, as studies have shown microstructural changes in white matter as well as cortical thinning in former professional soccer players aged 40 to 65. Yet, less is known about the effects of sub-concussive and repetitive hits in soccer.
The research group from Scotland used transcranial magnetic stimulation (TMS) to study a common marker for concussion called corticomotor inhibition, which manifests as a silent period in the signal from the instrument. The TMS findings ultimately indicate electrophysiological changes in the brain after hits to the head.
Additionally, the team used the Cambridge Neuropsychological Test Automated Battery (CANTAB) to assess cognitive changes in the brain. Within this computer-based test, the researchers could study reaction time, spatial working memory, attention switching, and rapid visual processing.
Twenty-three healthy amateur soccer players between the ages of 19 and 25 were recruited for the study. They excluded participants who had a previous brain injury involving loss of consciousness and a history of concussion in the past 12 months. The individuals were then given a series of baseline tests before moving onto the “heading” protocol.
This protocol involved heading a standard soccer ball twenty times over a 10-minute period. The balls were launched from a machine 6 meters away at roughly 24 miles per hour. They used a custom built accelerometer on the back of the participant’s head to measure the g-force from the impacts. The participants then repeated the baseline tests immediately after the activity and three more times at 24 and 48 hours, and finally at 14 days post activity.
They discovered increasing lengths of silent signals in the TMS, which indicated mildly significant increases in the corticomotor inhibition immediately after the activity. There was no significance at any other time points, however. They also observed higher error scores in spatial working memory cognitive test immediately after the activity, which was indicative of impairments in short-term memory. Additionally, they observed higher error in tests of long-term memory function immediately following activity. While no other cognitive tasks had significantly different results, the study did provide evidence of transient disturbances in both short and long-term memory. Even though the impairments from the sub-concussive impacts didn’t ever persist for a full day, these results represent the first evidence that headers immediately affect the brain.
The research team believes that increases in silent periods could be linked to increased GABA inhibitory activity, which might be a mechanism for the body to protect itself against minor injury. The increased corticomotor inhibition, however, has previously been associated with pathophysiology in brain damage and suggests a link between functional issues in the brain and overactive inhibitory neurons.
While the study is far from perfect in terms of design and significance of results, it hints at immediate brain changes that cannot be taken lightly. Further studies into the effects of sub-concussive hits in soccer, i.e., routine headers, must be undertaken. The specific types of headers and the actions that contribute to these changes should be studied in order to improve education on safe heading practices. Additionally, studies should look into the effectiveness of “soft” helmets that are becoming more common in soccer.
Today, we see entertainment, money, and/or temporary happiness as potential higher priorities compared to our brains. TBI’s (traumatic brain injury) like a concussion can cause detrimental molecular issues which can have short and long lasting effects on your brain and the rest of your body. I am going to write about how people are ignoring the facts of a concussion just so they can do what they want and be “successful” in their realm of work. I will first talk about how concussions can vary and you can manipulate your concussion, and secondly, I will talk about the second impact syndromes well as the effects of a concussion short and long term and how TBIs can lead to higher probably chances of issues like suicide.
As a professional athlete like Tom Brady or Canelo Alvarez, the last thing they want to do is sit out because of a concussion. For Brady, his team relies on him, he is their QB, and for Alvarez, he is practically fighting for himself but he knows if he fights he gets paid regardless and even more if he wins. These men will sometimes do whatever they need to do to make sure their involved in their sport and that may lead to providing false information on any concussion or TBI they have had. I encourage you to read up on one football players perspective on concussions found here. People today impact themselves in so many ways and the way these two men do it is through physical contact to their bodies and most importantly their brain. These men may make a lot more than the average guy, but they simple are doing their job. Their career, and unfortunately their physical degradation gives us entertainment all throughout the week on television. These men most likely also get joy and happiness through their sports, but they are missing huge key facts that concussions can cause short and long term issues as well as what happens when you don’t properly heal from a previous concussion.
Concussions commonly lead to rapid onset of short-lived impairment of neurological function that resolves spontaneously. At the molecular level hours after the concussion/TBI, hypometabolism occurs via decreased amounts of ATP, NADH/NAD, and N-acetylaspartate and this can occur up to months after a moderate or severe TBI. This gives evidence along with a high calcium influx that sets the stage for another severe brain injury after a repeated concussion—described clinically as second impact syndrome. In a general sense, symptoms and signs may evolve over several minutes to hours. Some short-term issues involved include: headache, foggy feeling, behavioral and emotional symptoms, slowed reaction times and insomnia.
According to Concussion Foundation, 87 of the 91 former NFL brains that were in a study had a progressive neurodegenerative disease called Chronic Traumatic Encephalopathy. This disease has symptoms of memory loss, confusion, impaired judgment, paranoia, and much more. The tau protein in the brain gets misfolded and causes build ups throughout the brain which cause neurons to die slowly. Another major issue found from concussions is their link to suicide. According to Canadian Medical Association Journal, someone who encounters just a mild concussion is three times more likely to commit suicide than someone who hasn’t had a concussion. Regardless of short or long term issues, concussions aren’t going anywhere soon and we as society need to be more informed on what they can do to your health over a lifetime.
Concussions: Science Says They’re a Big Deal
When I visited the movie theatre last fall to see Concussion, I expected to receive a dose of entertainment, but I instead received a dose of reality. It told a true story about a forensic pathologist, Bennet Omahu, handles the autopsy of Mike Webster, former NFL player for the Pittsburgh Steelers. After close examination of the NFL player’s brain, he discovers that there is evidence of severe brain damage, which contrasts with the individual’s otherwise healthy body, so Omahu concludes that the death is due to chronic blows to the head, a disorder he identifies as chronic traumatic encephalopathy (CTE).
Now this movie contains action, drama, romance, and thrill, but it,arguably, more importantly sheds light on the dangerous effects of concussions.
According to WebMD, a concussion is a type of traumatic brain injury caused by a blow to the head or body, a hard fall, or basically anything else that shakes the brain inside the skull. Concussions are a unique injury, because the damage cannot necessarily be obvious. A concussion causes normal functions in the brain to malfunction. The people most susceptible to getting a concussion are athletes, with football, boxing, and soccer having higher rates of concussions.
Symptoms of concussion include headache, nausea, fatigue, memory problems, sleep disturbances, and mood dysregulation, according to the Brain Injury Research Institute. In many cases signs of a concussion appear right away, but they may not appear until a couple days later. This makes diagnosing a concussion difficult, and it leads to additional risks if it is not treated immediately post-impact.
More research on the long-term effects of concussions has investigated the dangers of repeated concussions than the lasting complications of a single concussion. Research has concluded that repeated concussions are especially damaging in regards to long-term health. Some long-term consequences of repeated concussions include
- Cognitive impairment
- Anxiety disorders (PTSD)
- Learning interference (spatial learning)
- Depression
- Motor dysfunction
- Memory deficits
- Alzheimer’s Disease
- Mood Instability
When I was watching Concussion, I was amazed to see how seriously Webster’s life fell apart. We was pictured suffering from self-mutilation and homelessness, and he ended up dying alone. Realizing that this is the experience for many people due to CTE makes the severity of concussions seem much more real.
This understanding directed my curiosity to learn more about concussions and how they affect the brain. According to a 2014 article in Neurosurgery, brain injury leads to damaged axons (part of the neuron that transmits a signal to another neuron).

The axons get stretched so that calcium and sodium ions enter into the cell, and this leads to excess excitatory neurotransmission. The mitochondria goes into hypermetabolism to try to restore the balance and ultimately goes into hypometabolism because it has entered an energy crisis. Concussion also leads to an accumulation of abnormal proteins in the brain.
The Sports Concussion Institute has developed a graduated “Return to Play” protocol that details the rehabilitation stages a player must go through to return to playing their sport after a concussion. This management plan has been challenged by the “Return to Learn” protocol, which insists that players must be reintegrated to academics before athletics after a concussion, according to the Brain Injury Association of America.
It is advancements like these that will help individuals properly heal after a concussion before being back on the field with the risk of receiving another one.
I can’t imagine how hard it would be to get a concussion as a high school athlete. I would want to keep playing, no doubt. Protecting my brain for the sake of my long-term health wouldn’t be the first thing on my mind. Then to think of a professional athlete who might have devoted teammates and millions of fans depending on him or her, that would be even trickier.
As a culture, we need to balance our passion for competition with concern for future health. This will be a step in the right direction of enhancing lifelong health and reducing diseases that get in the way.
Return-to-Play and Second Impacts
In the past, there has been little research done on concussions and what is actually going on in the brain, until recently. Neuroscience research has grown and with that the research on concussion has taken a keen interest. The importance of finding the effect concussions have on the brain is a major contributing factor on how treatment should be done and how the Return to Play (RTP) protocols should be handled in order to properly heal and avoid a secondary impact.
The standard misperception on what happens as a result of a concussion is neuronal (cell) death occurs which causes the symptoms. However, what actually goes on in the brain is a change in the biological pathway. What is thought to occur is axonal damage of the neurons results in an influx of sodium and calcium and efflux of potassium. Compensation occurs by way of oxidative stress within the mitochondria and an ATP need increase causes hyper-metabolism. Axonal transport is affected as well. Later, hypometabolism occurs. This is where the problems with most RTP protocols are. A longer duration of time is needed for this phase of the injury to heal. It is essential to avoid a secondary impact during hypo-metabolism. The brain is low on energy already and a second impact would cause it to go into hyper-metabolism again. Lastly, accumulation of abnormal proteins occurs along with inflammation.
In order to avoid concussions, a change needs to be made. Within secondary school, a change can be made in the Return-To-Play (RTP) protocol with an addition of Return-To-Learn (RTL). In California, there are schools which implement completion of the RTL program before starting the RTP. This allows the student to catch up with school work that has been missed while they had their concussion and lessens the chance of the individual receiving a secondary impact before completely healed. Another change that can be made is the awareness of concussion occurrence at a younger age and education to coaches of primary school sports. Adults’ and parents’ awareness of concussions are shown within a high school, but often it is not thought about with elementary or middle school.
One problem faced when dealing with concussions is the awareness of the severity that can result in no matter the age, how hard the impact, and if not healed properly. Unmyelinated neurons are more susceptible to injury, children are growing and have a higher percentage of unmyelinated neurons and therefore, may be more prone to concussions. Although children may heal faster, it is important to be aware children can give and get concussions as well. Another problem faced is the thought that it must be a hard impact in order to receive a concussion. This is not true; individuals can receive multiple small impacts and get a concussion. Lastly, if the concussion is not healed properly and a second impact occurs, it will result in a worse injury than initially. In other words, it is better to sit out and wait to be healed than get in the game too early and set yourself further back.
Concussions: Not Just an Excuse to Miss School
Concussions are a not well-understood invisible injury that has no boundaries on who it can affect. A concussion may be caused by a blow, bump or jolt to the head, or by any fall or hit that jars the brain. This invisible injury disrupts the way the brain normally works by affecting mental stamina, as the brain must work longer and harder even to complete simple tasks.
Recently, researchers have figured out the neurochemical cascade that occurs in the brain after a concussion:
- There is depolarization in the cell and release of high amounts of excitatory neurotransmittors.
- Potassium is brought out the cells and Calcium is rushed in causing an imbalance (Hypermetabolism).
- Increased activity of ATPase and a decreased production of ATP (Energy Crisis).
- Axolemmal disruption, axonal swelling and possible apoptosis.
- To much stored Calcium, no ATP for energy, no activity Hypometabolism).
This cascade shows us why patients are very tired, but also that sleep is very important to a concussed person. The Hypometabolism stage shows us why second impact syndrome is so bad, because if you receive another concussion in this state there are no chemicals of energy left to start this cascade over again.
Concussions are serious brain injuries that have a significant influence on the brain’s ability to function at its normal capacity. The key to recovery from a concussion is both physical and mental rest, followed by a gradual progression back to activity, both in athletics and in the classroom.

Concussion symptoms can have a significant impact on classroom learning and schoolwork. Physical symptoms may interfere with the student’s ability to focus and concentrate, while cognitive symptoms may impact the ability of the student to learn, memorize and process information, as well as keep track of assignments and tests. Struggles with school work may worsen the frustration, nervousness and irritability that were originally caused by changes in brain chemistry.
No two concussions are exactly the same so individualized treatment is necessary. Developing brains are highly variable; so one student’s symptoms may be completely different, and therefore, some students may need to miss school to help heal for varying amounts of time, while others will be able to continue their work with some accommodations.
Nationwide Children’s has come up with a 5 step plan for teachers to understand when helping a concussed student through school work.
- No School: Rest with no activity, screen time and healthy meals are key to begin the healing process
- Half-day Attendance with Accommodations: Accommodations may be limited homework and reschedule tests.
- Full-day Attendance with Accommodations: Accommodations may be breaks in between classes.
- Full-day Attendance, No Accommodations. No activity is allowed yet, full class load is allowed.
- Full-day and Extracurricular Activities.
A concussed student needs to hear from educators that they understand what a concussion is and what the student may be experiencing. The student needs reassurance that he or she will not fail classes because of missed school days and homework. This sympathy, understanding and consistency from all parties involved will help to decrease stress, and in turn, help with recovery.
We Need to Let People Heal From Concussions
Concussions can cause long lasting neurological problems. In extreme cases head trauma (even sub-concussive) can lead to chronic traumatic encephalopathy. This neurodegenerative disease has horrible symptoms, memory loss, disorientation, violence, social issues, depression, even suicide.
When I started doing research on CTE this week I was shocked. I saw story after story of successful, motivated people falling victim to this horrible disease. It would their lives. All because of a history of concussions.
So what can we do to prevent brain injuries? We could stop doing activities that result in concussions.
Sadly, that is impossible. Even if it was possible to convince people to stop playing contact sports like football, wrestling and even soccer; car crashes and other accidents would still exist and people would still get head trauma.
Since it is impossible to completely prevent concussions. We need to do a better job treating them and educating people on the importance of recovering from concussions.
Currently there is no conclusive biomarker such as a blood test that can tell if someone has a concussion. However, it likely that this will be possible in the future. For now, medical professions must diagnose concussions by symptoms described by the patients.
This system has a problem. Athletes and students with concussions face pressure to keep up in school and return to playing sports as soon as possible. This is problematic because it doesn’t give them time to heal. Ideally after a concussion a person should not just abstain from TV and sports but should really limit reading, intense problem solving, and studying. Sadly, this is not feasible for the vast majority people.
We need to prioritize our health and let people recover from concussions to prevent permanent neurological damage. Having people try to continue normal school or work activities with a concussion is like asking someone with a broken ankle to go run a mile. It will just make the healing process more painful and difficult and may end up making the injury worse.
Another reason to let people heal is second impact syndrome. This condition is caused by multiple concussions occurring in a short period of time. It can cause permanent disability or even death.
We need to let people recover after concussions and be more cautious in letting people return to normal activities. If people can’t avoid getting concussions we need to let them heal, or there could be permanent neurological consequences.
Concussions: Should We Take Them More Seriously?
As the world of science has expanded, concussions have begun to be understood more. Even when I was in high school, concussions were not that big of a deal. Now, concussions are treated with a lot more care, as they should be. It was until recently that I truly understood just how serious a concussion can be. Having had two concussions myself, I now realize I did not take them as serious as I should have.
Concussions are essentially a hard blow to the head. But, the underlying mechanisms that go on after the hit is what causes all of the symptoms such has headaches and nausea. At the molecular level, many non-specific depolarizations start to occur after an impact. As the neurons begin to fire, there is a release of excitatory neurotransmitters, which is followed by an efflux of potassium. Many ionic membrane pumps begin to go into overdrive, trying to retain homeostasis. This is coupled with an increase need for ATP due to the extra work of the ionic pumps. The cells are launched into hyperglycolysis as they try to keep up with the energy demands. After a concussion, the cell membranes also become “leaky” resulting in an increase of calcium inside of the cell. This also results in more action potentials, and contributes to the increased energy demand.

Eventually, the energy demand becomes too much and results in a decrease in ATP production. This leads to a hypometabolism state, which is in my opinion, the key part to understand in a concussion. If an area of the brain is unable to produce the energy it needs in order to meet baseline needs, then the brain obviously needs to rest. This is why doctors recommend as much rest as possible immediately after a concussion. This includes: no sports, no screen time, and less school time.
Taking a physician seriously with all of their recommendations for a concussion can be difficult. How can a person just not go to school for a few days? The hypometabolism that results from a concussion needs rest in order to attain normal order again. The brain will not be able to rest as efficiently if a person is trying to listen to a lecture or do homework. Without the needed rest, the brain is more susceptible to a second concussion, which would result in going back to square one for recovery. This is why it is very important to take the recommended time to rest in order to allow a speedy recovery and to get back to normal everyday life.
After learning how important rest is for concussion recovery, I know that I did not take the needed care after I had mine. This can be scary, because I may have left my brain to be more susceptible to re-injury or possible some other effects later in life. So, my message to you: give your brain the rest it needs after you experience a concussion, that really is the best “medicine” for it.