Picture 1: Addiction affecting the brain.
Addiction is a difficult disorder both mentally and physically for the individuals, but also for the people around them. Additionally, it has been found to have effect on structures within our brains. But what is addiction, or more specifically substance use disorder (SUD), it has been defined as “a drastic and chronic relapsing disorder characterized by difficulty in limiting drug intake, showing high motivation for drug use, and pursuing drug-taking despite negative emotional and physiological experiences”[1].
How does addiction affect the brain?
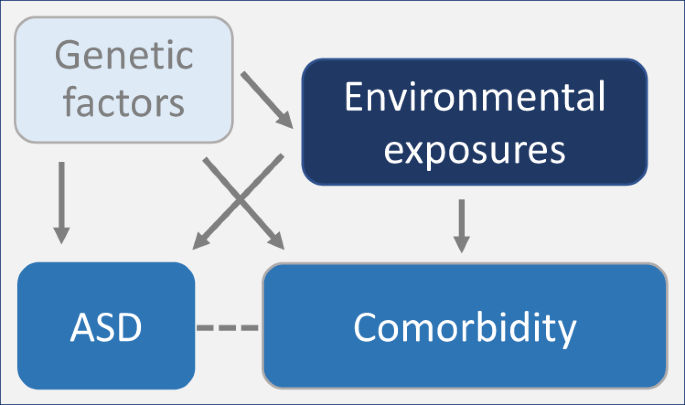
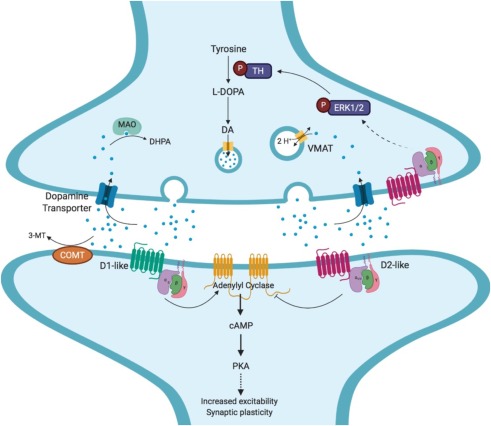
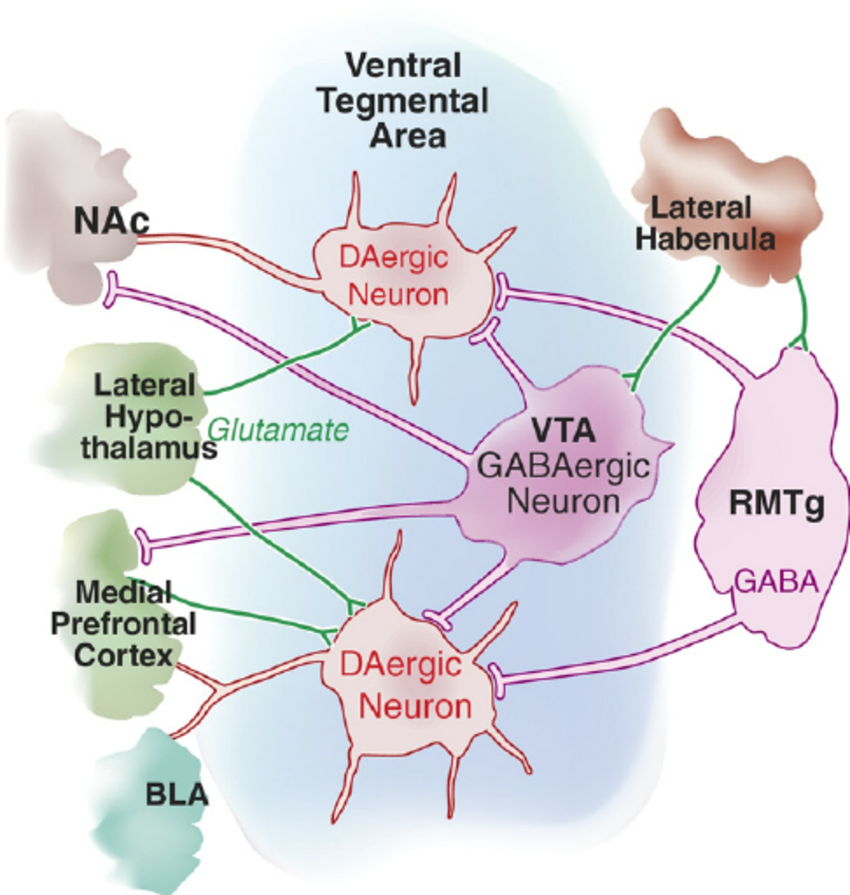
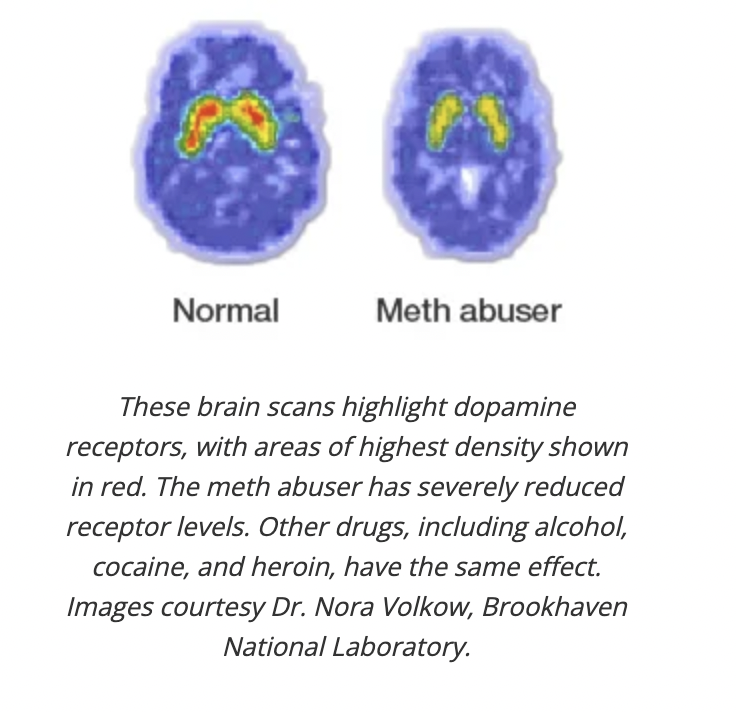
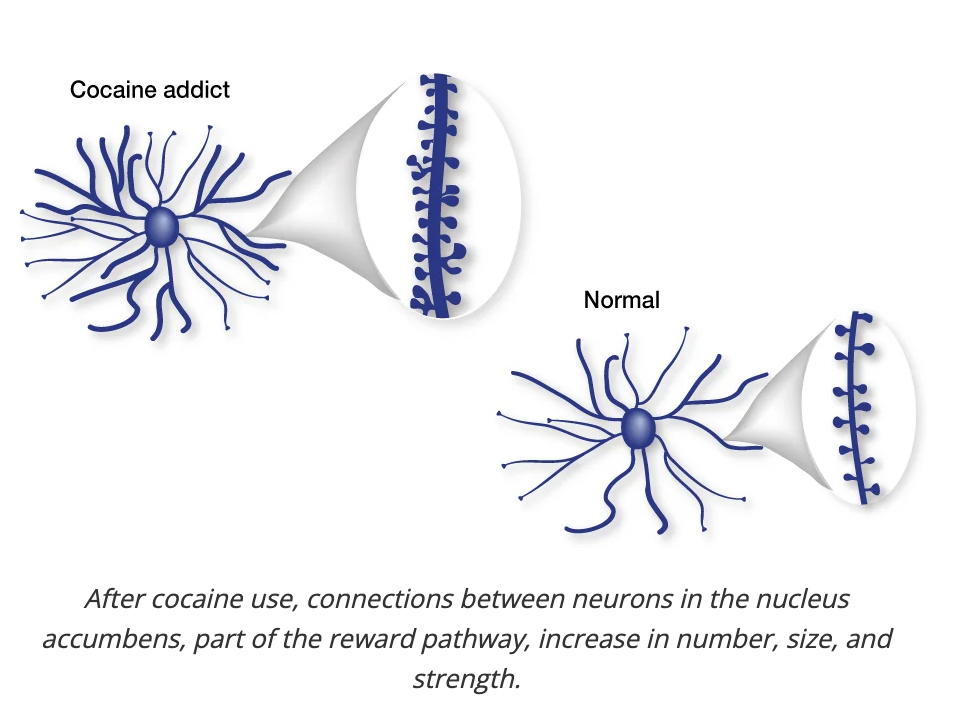
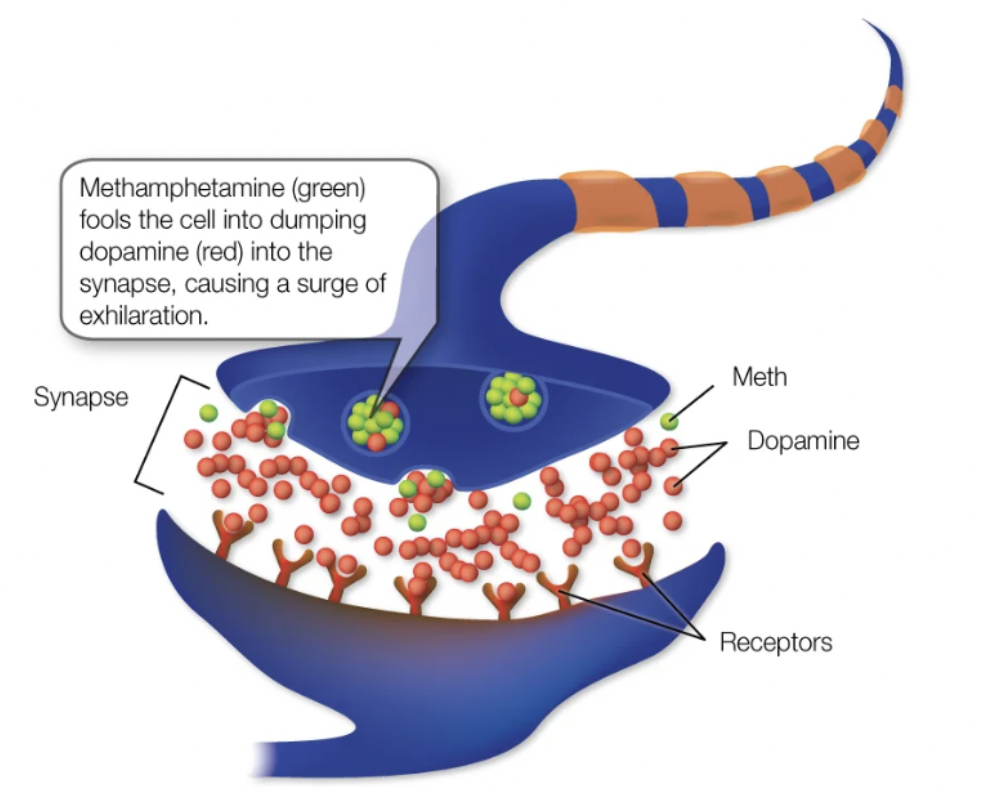
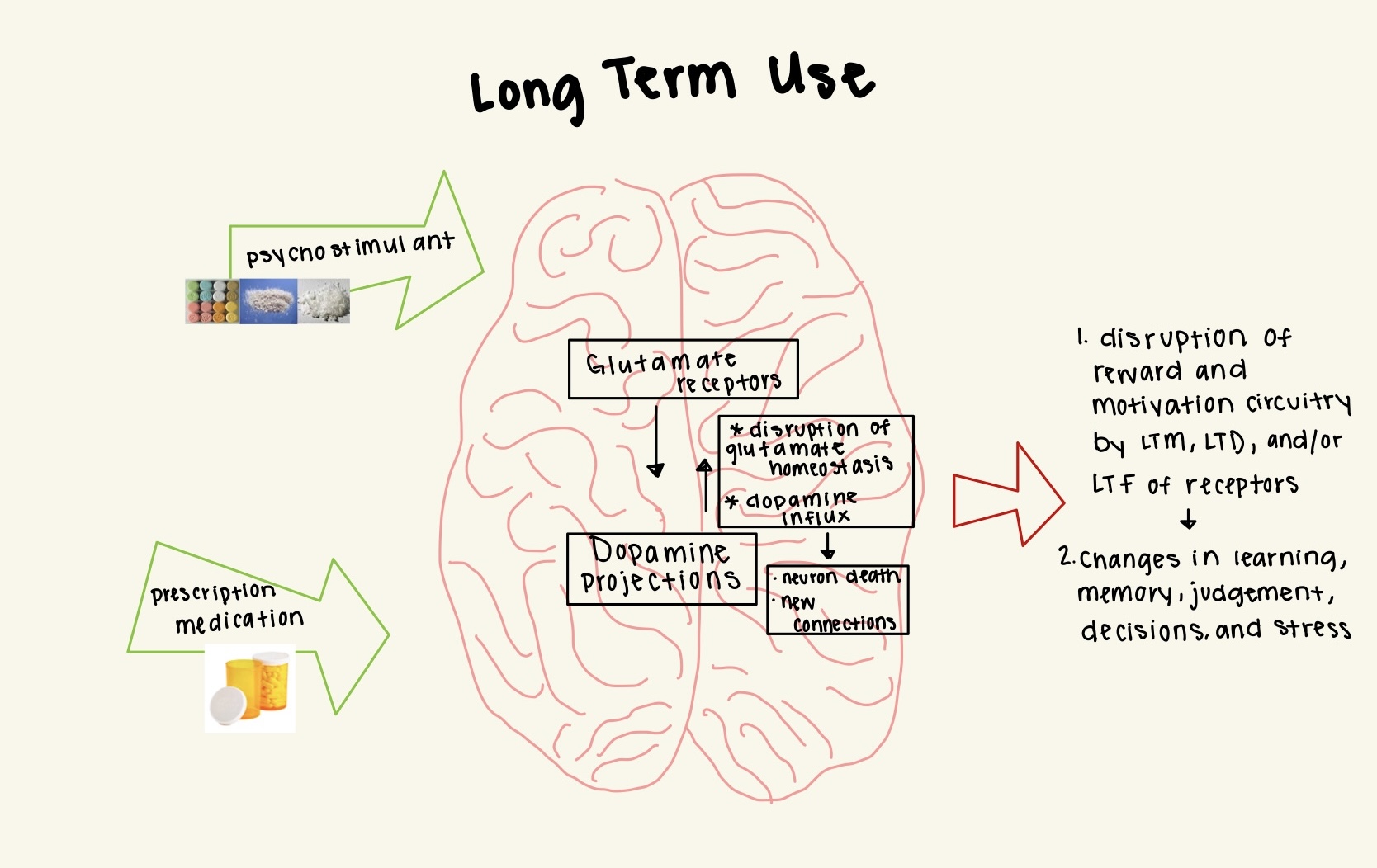
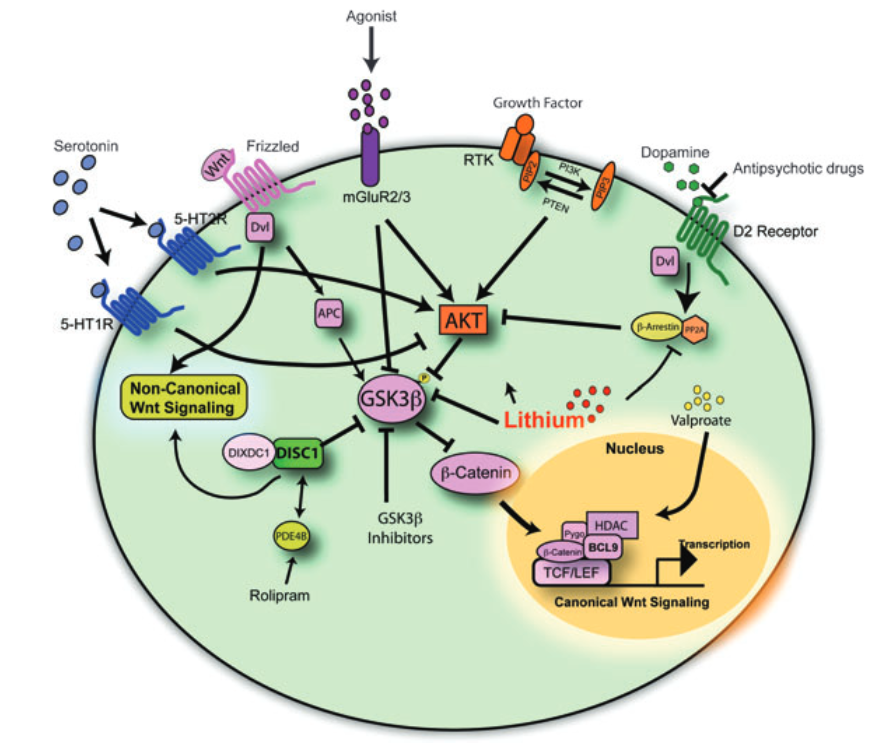
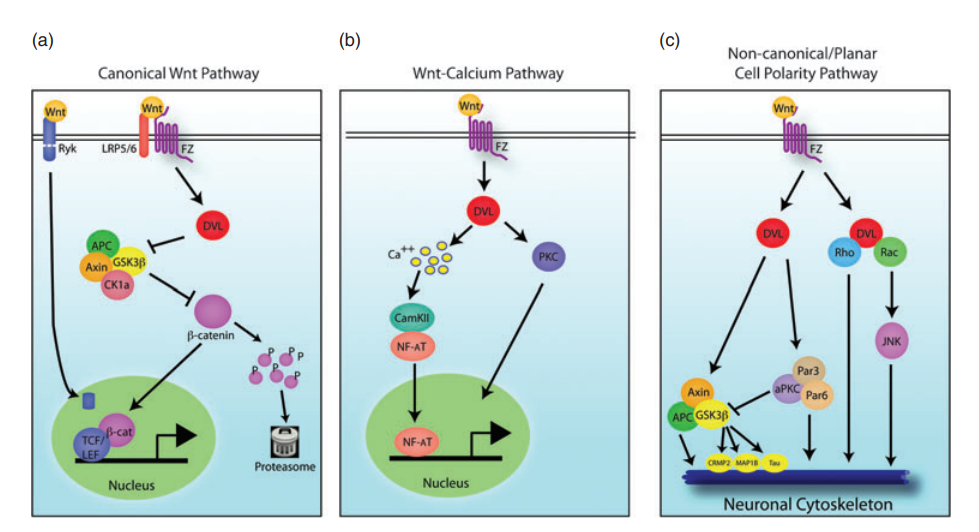
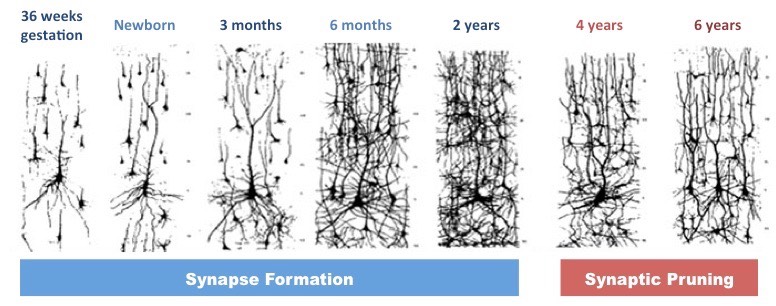
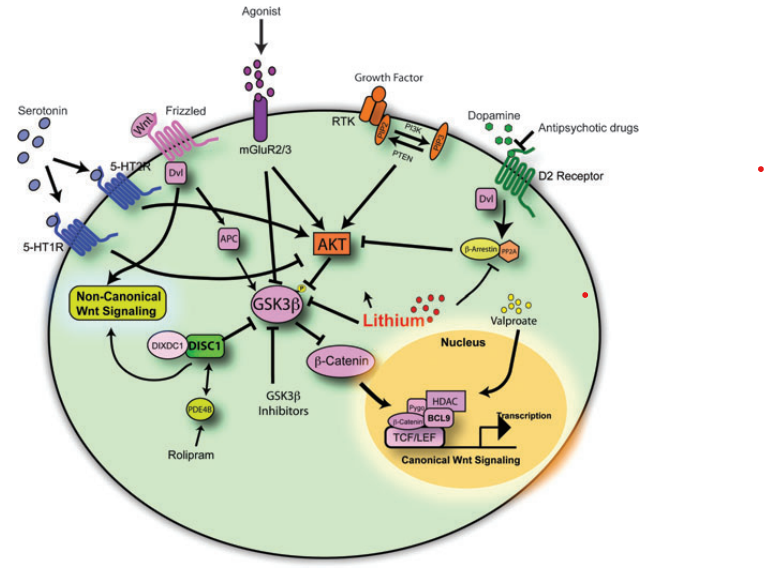
The reward circuits are a part of all the motivated behaviors that are related to both natural and drug reinforcers and are therefore this brain circuit plays a bigrole in addiction. Prolonged drug abuse causes dysregulated functional connectivity in the brain that alters receptor and transporter expression for monoamines and changes the strengths of the synapses (Figure 1). This leads to more frequent neurotransmitter synthesis and release in various part of the reward circuit[2]. These impairments contribute to the behavioral and cognitive impairments in people that suffer from addiction. There are several brain regions connected to the reward circuit, these include the ventral tegmental area (VTA) and the nucleus accumbens (NAc).
Glutamate is the most excitatory neurotransmitter in the central nervous system, as well as having a role in the brain regions that are connected to the reward circuit which makes glutamate a central neurotransmitter when understanding drug use disorders.
 Figure 1: Synaptic plasticity, increase in neurotransmitter release and/or number of postsynaptic receptors available.
Figure 1: Synaptic plasticity, increase in neurotransmitter release and/or number of postsynaptic receptors available.
The increase in catecholamines, primarily dopamine, leads to more neurotransmission that leads to synaptic plasticity. In relation to addiction the synaptic and memory theory plays a role in understanding the changes that happens within brain. Learning happens thought various synaptic mechanisms cause changes in the connection that happens between neurons[3]. When the synaptic mechanisms are changed, and the brain learns new ways to function as a response to the drug use, it changes the mechanism within the brain.
The role of empathy
Picture 2: showing empathy.
After seeing the effects that drug abuse have on the brain, and the change in structures within the brain, can behaviors by individuals with these disorders be better understood? Empathy might play a significant role for people dealing with these disorders, and that coming from the people around them if its health professional or family members it can be crusical in recovery. There is a lot og negative stigma around drug use disoders, and that causes a lack of empathy, because it is hard to understand why an indivdual would pertain to certain behaviors. Looking into the physical changes in combinations of understanding why someone develop the disorder, can lead people to have more empathy for the individuals that are struggling with these disorders.
The causes of addiction can be many, such as comorbities, trauma, stress, etc., and the relation might give a better look into the development of drug use disorders. As for cormorbidities, mental health disorders and somatic disorders can play a role in why someone develop the disorders. Depression is the most prevalent for the mental health disorders that comorbid with drug use disorders[4], and these can be risk factors for developing the substance use disorders. In order to create a better understanding, and for people to improve their empathy for people with these disorders, might be the indivudals differences, and the background to why they developed the disorder.
Bibliography
[1] Mozafari, R., Karimi-Haghighi, S., Fattahi, M., Kalivas, P., & Haghparast, A. (2023). A review on the role of metabotropic glutamate receptors in neuroplasticity following psychostimulant use disorder. Progress in neuro-psychopharmacology & biological psychiatry, 124, 110735. https://doi.org/10.1016/j.pnpbp.2023.110735
[2] Mozafari, R., Karimi-Haghighi, S., Fattahi, M., Kalivas, P., & Haghparast, A. (2023). A review on the role of metabotropic glutamate receptors in neuroplasticity following psychostimulant use disorder. Progress in neuro-psychopharmacology & biological psychiatry, 124, 110735. https://doi.org/10.1016/j.pnpbp.2023.110735
[3] Mozafari, R., Karimi-Haghighi, S., Fattahi, M., Kalivas, P., & Haghparast, A. (2023). A review on the role of metabotropic glutamate receptors in neuroplasticity following psychostimulant use disorder. Progress in neuro-psychopharmacology & biological psychiatry, 124, 110735. https://doi.org/10.1016/j.pnpbp.2023.110735
[4] United Nations Office on Drugs and Crime (March, 2022) Comorbidities in drug use disorders. Commission on Narcotic Drugs, 65th session. Retrieved from https://www.unodc.org/documents/drug-prevention-and-treatment/UNODC_Comorbidities_in_drug_use_disorders.pdf on 2024, March 12
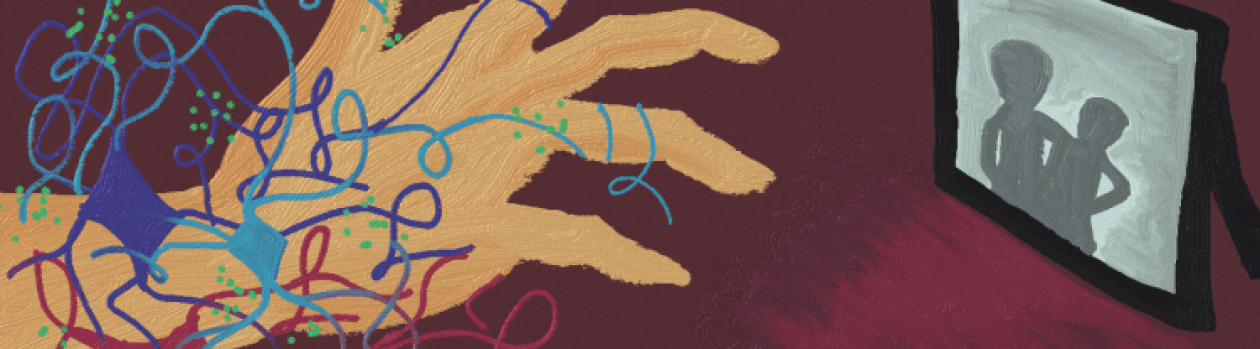



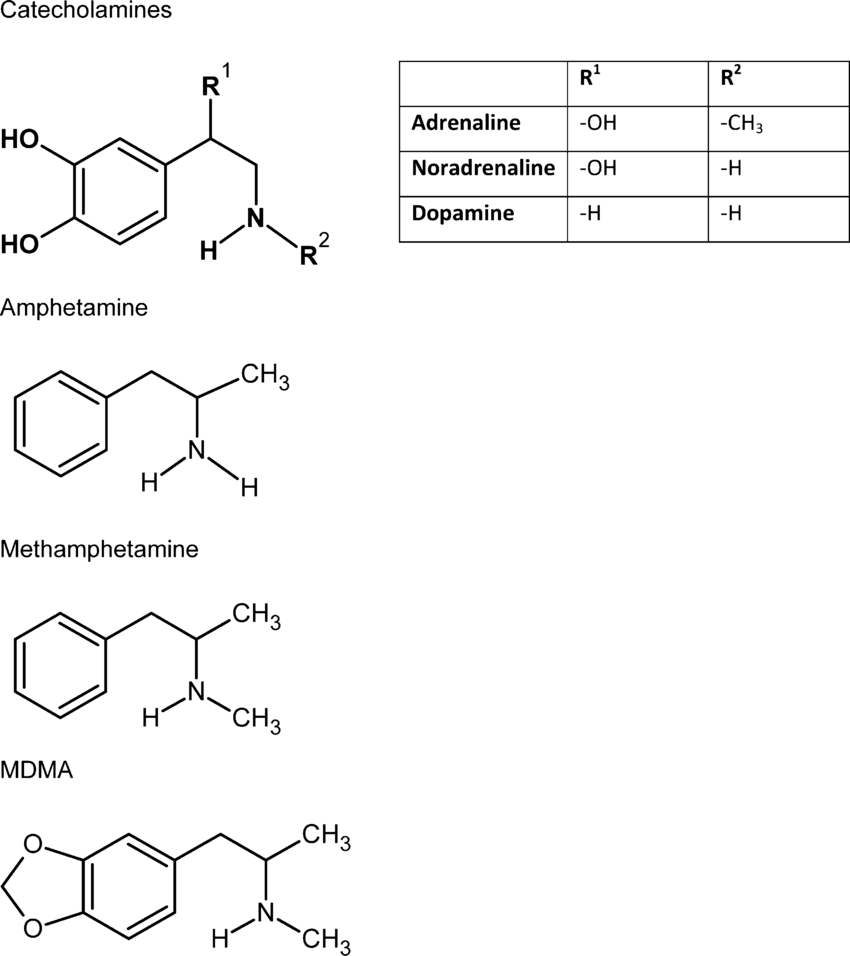 Figure 1. Psychostimulant structure compared to catecholamine neurotransmitters (2).
Figure 1. Psychostimulant structure compared to catecholamine neurotransmitters (2).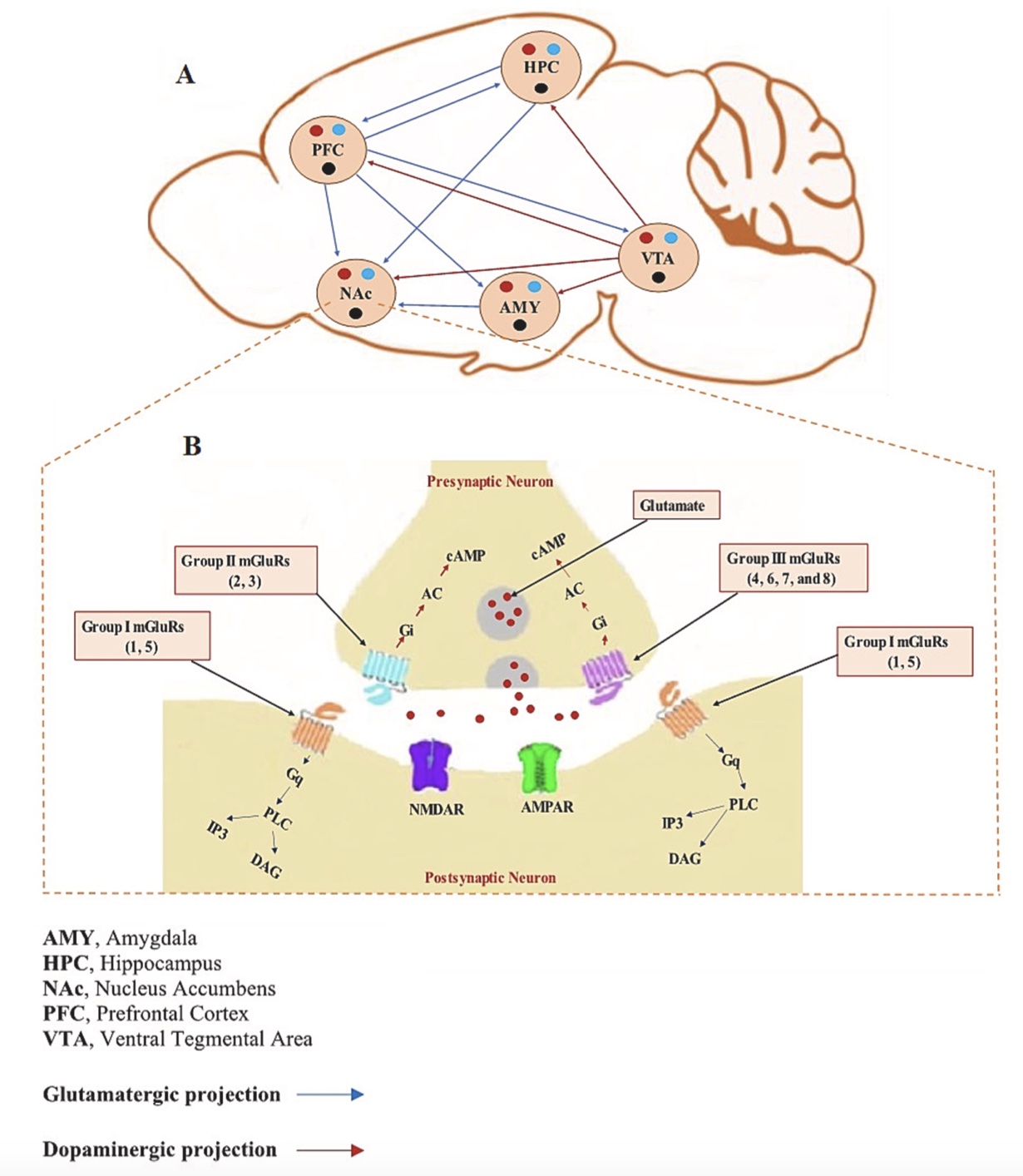






:max_bytes(150000):strip_icc():format(webp)/schizophrenia-sign-symptoms-5095511_final-57a52853a10c4edcb4bd6a3b31f041ea.jpg)




 P
P