It’s fairly well known that obesity can lead to an increased risk for numerous different health outcomes, such as type 2 diabetes and cardiovascular diseases. Obesity also causes a state of constant low-grade inflammation in the body, which in turn has it’s effects on the brain as well that people often don’t realize. Many thing’s go wrong in the body and brain that contribute to obesity, primarily an imbalance of energy homeostasis and hunger cues.
What’s Happening in the Brain
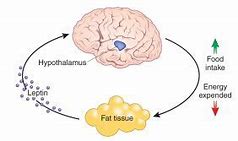
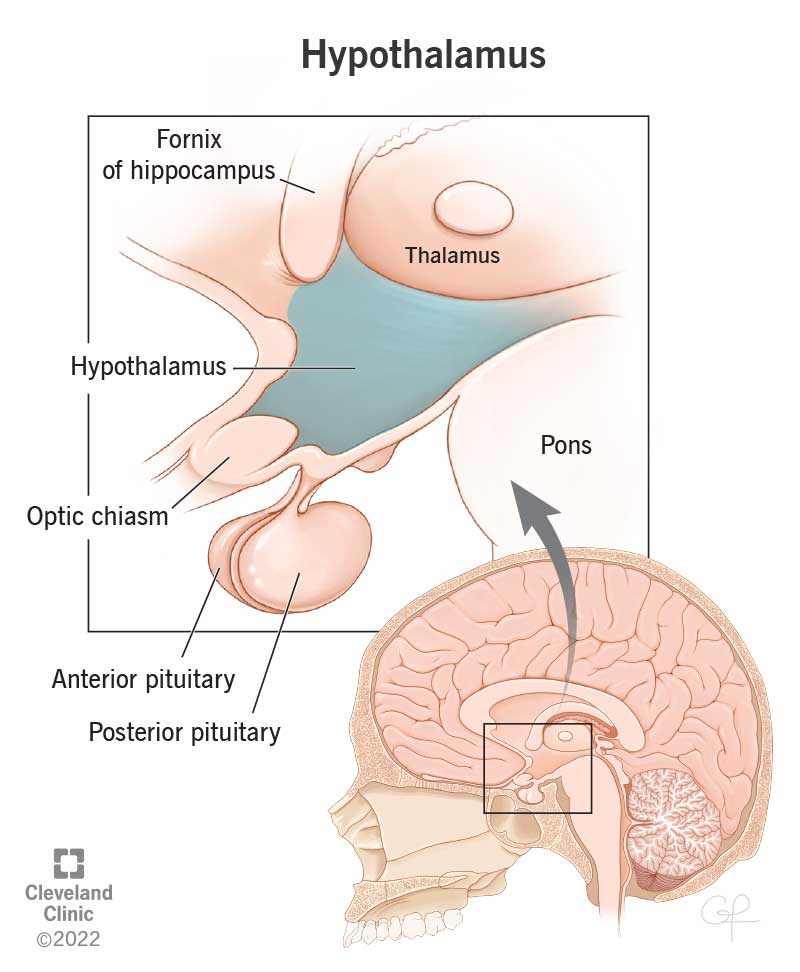
The hypothalamus region of the brain controls several endocrine functions that take metabolic feedback and regulate energy homeostasis. Basically, the hypothalamus will give signals to either increase or decrease hunger and energy use in response to the signals the body sends to the hypothalamus. Obesity can occur due to disorders of the hypothalamus, such as Prader-Willi syndrome. This is an inherited disorder that causes the hypothalamus to not recognize the sensation of being full when eating. This causes a constant urge to eat, and puts you are risk for obesity.
The Melanocortin System
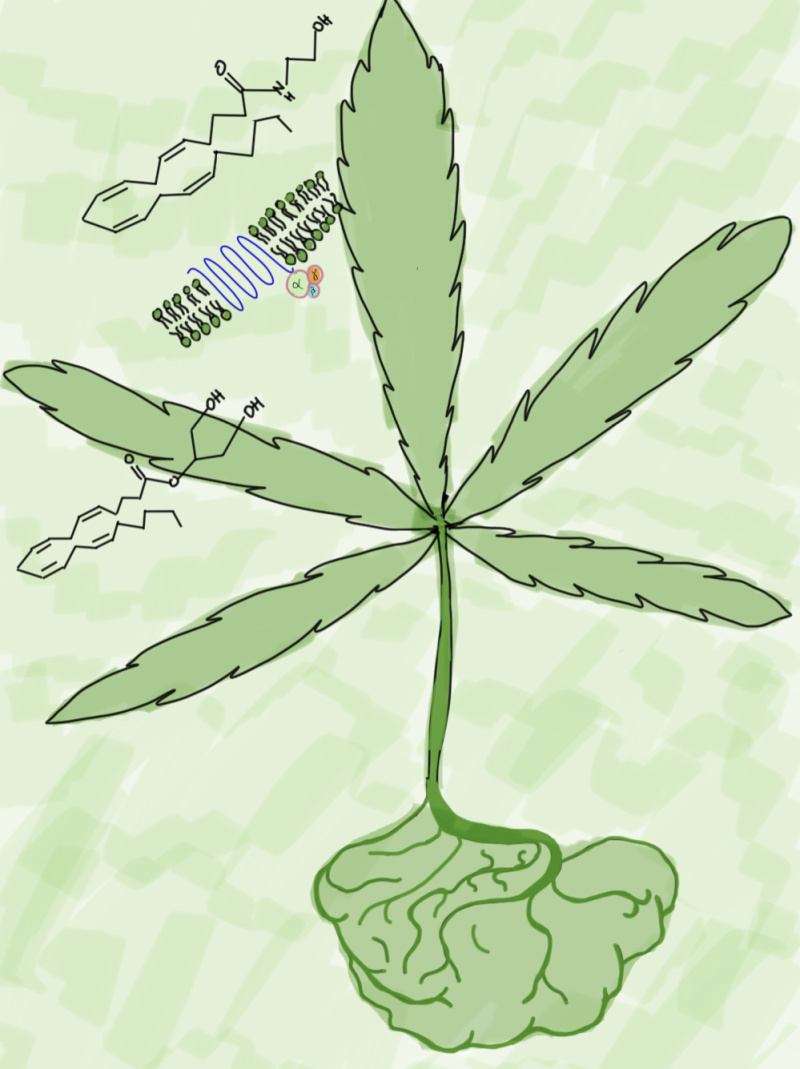
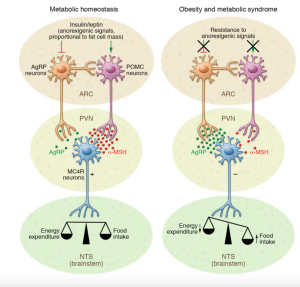
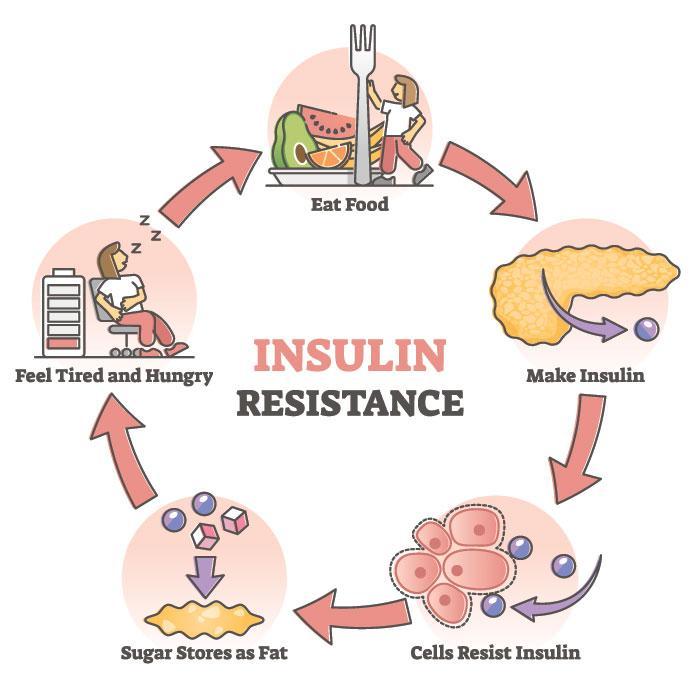
The main player in this regulatory function is the melanocortin system. Insulin and leptin circulate the body in levels that are proportionate to the amount of adipose (fat) tissues, and the nutritional status of the body. These molecules bind to receptors in the melanocortin system and will decrease food intake, and increase energy usage.

In a healthy brain these cues are in balance, leading to a balance of energy usage and food intake. In obesity it’s been studied that there is a dysfunctional melanocortin system, leading to an increase of food intake and decreased energy usage.
Dietary Fats
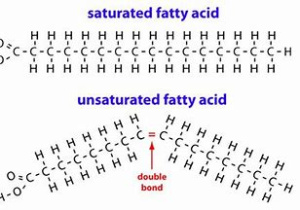
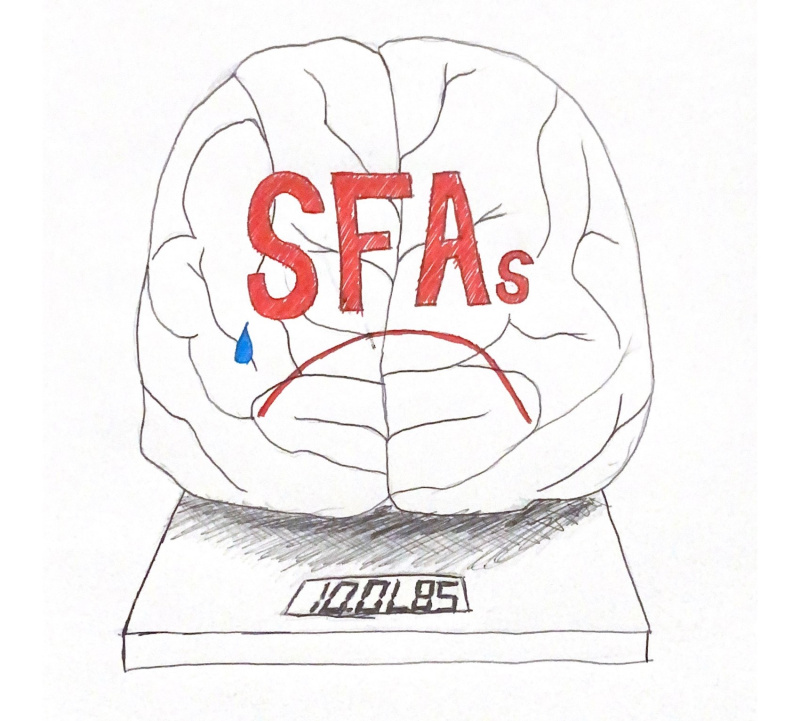
Surely you’ve been told to eat the ‘right’ foods, and that fats usually aren’t those right foods. And maybe you’ve heard of ‘good’ fats and ‘bad’ fats, but what makes those different? The main two groups are saturated fatty acids (SFAa), and unsaturated fatty acids.
Saturated fats the ‘bad’ fats. They are typically solid at room temperature, meat and dairy products are the main dietary sources of these. Their structure consists of only single bonds, and have the maximum amount of hydrogen atoms in their structure. These fats are known to raise both good and bad cholesterol in the body, raising the risk of cardiovascular and other diseases.
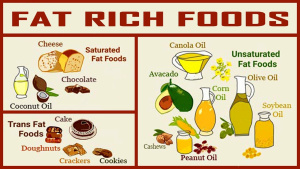
Unsaturated fatty acids are the ‘good’ fats. These are more complex molecules, consisting of double bonds that cause bends in their chain. These fats are typically liquid or fluid like at room temperature. Common sources of these are oils such as vegetable or canola oil, nuts, and fish. These fats typically raise the level of good cholesterol in our body.
Effects of Fats in the Body and Brain
Studies have been done in rodents about the effects of certain fats on the hypothalamus. A diet with high amounts of SFAs have been shown to increase hypothalamic inflammation in days, while mono-unsaturated fatty acids did not compromise and hypothalamic function. SFAs have also been shown in these studies to cross into the brain and accumulate in the hypothalamus, where they block insulin and leptin signaling, and will disrupt the melanocortin system. It’s recommended that about 10-30% of our calorie intake should be fats, although only about 5-10% of caloric intake should be saturated fats.
References
- https://my.clevelandclinic.org/health/articles/22566-hypothalamus
- https://www.sciencedirect.com/science/article/pii/S2212877821000466
- https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fat/art-20045550
- “Hypothalamic Inflammation in Obesity and Metabolic Disease” A. Jais



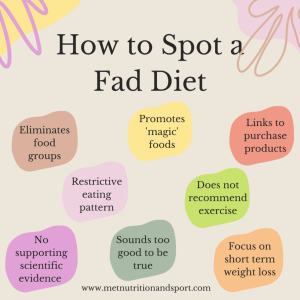 We have all heard and seen that the south beach diet, the keto diet, the 3-day diet, the juice diet, and many more of these types of diets are recommended for fast weight loss, but this is 100% wrong. These diets are all called
We have all heard and seen that the south beach diet, the keto diet, the 3-day diet, the juice diet, and many more of these types of diets are recommended for fast weight loss, but this is 100% wrong. These diets are all called 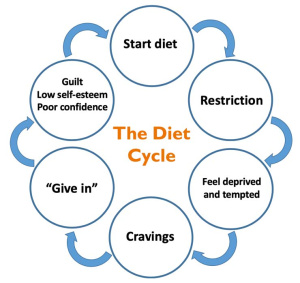
 The beginning of the new year brings up this idea of new years resolutions. January is a very common month to see these new diet trends make an appearance as well as weight loss products. In the United States alone,
The beginning of the new year brings up this idea of new years resolutions. January is a very common month to see these new diet trends make an appearance as well as weight loss products. In the United States alone, 
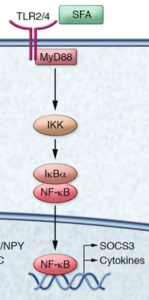
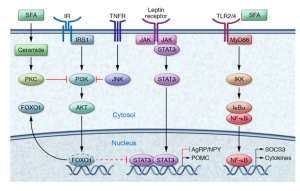
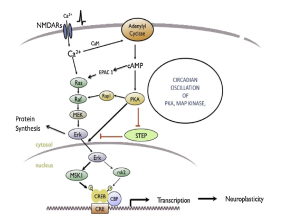
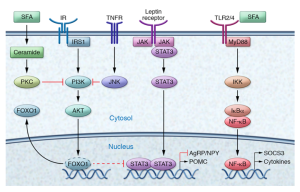 This image shows the many pathways involved in metabolic inflammation of the hypothalamus. This image just shows how complex inflammation is and how many moving parts there are. Inflammation of the hypothalamus affects many different cells types such as microglia, astrocytes, oligodendrocytes, and macrophages. Understanding the way that all the pieces fit together can help understand that obesity can be connected to the brain and help ways to properly treat obesity.
This image shows the many pathways involved in metabolic inflammation of the hypothalamus. This image just shows how complex inflammation is and how many moving parts there are. Inflammation of the hypothalamus affects many different cells types such as microglia, astrocytes, oligodendrocytes, and macrophages. Understanding the way that all the pieces fit together can help understand that obesity can be connected to the brain and help ways to properly treat obesity.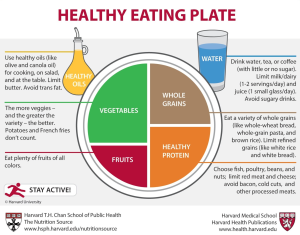 Proper weight loss is complex and there are many factors that play into it. Each persons body is different and needs different levels of nutrients so it is essential to not follow other peoples diets exactly. Looking at the food pyramid and
Proper weight loss is complex and there are many factors that play into it. Each persons body is different and needs different levels of nutrients so it is essential to not follow other peoples diets exactly. Looking at the food pyramid and 




 pexels.com stock photo by Darya Sannikova
pexels.com stock photo by Darya Sannikova