Night time light exposure is seemingly common. From working into the night hours to binge watching your favorite Netflix series, we are constantly bombarded with blue light exposure at night. The exposure to constant light does not come without a cost. Humans were made to function and follow an intelligent circadian rhythm. One that allows us to feel energized and ready to take on each day, and ready for a good night’s rest at night. Our circadian rhythm is highly regulated through the use of light. With light in the morning helping us to suppress melatonin and wake up, while in darkness in the evening to help us get tired before bed. What happens when we disrupt this natural rhythm? How does our sleep change and body respond?
What’s the Cost?
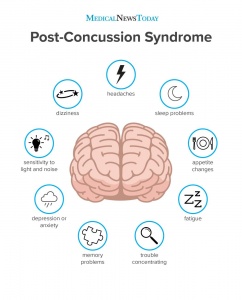
During the night, humans undergo processes of REM and NREM sleep. However, if this is fragmented, daytime functioning is impaired and increased sleepiness occurs. This has further implications on human health including disruption of metabolism, cardiovascular function, mental health, and even cancer risks. In particular, artificial light at inappropriate times, specifically light at night and exposure to light from mobile devices like phones, computers, and tablets is known to cause this disruption in addition to poor performance, insomnia, emotional disturbances, and gastrointestinal issues.
It has been shown that short-wavelength light (470nm or lower) is associated with a decrease in melatonin, reduction in reaction times, and depression in sleepiness, as well as changes in EEG power in the delta-theta frequency range. The cognitive effect of light is increased in alertness. Disruptions in our natural circadian rhythm can cause disruptions in our ability to have REM sleep, which is needed for memory consolidation and learning abilities.
Dim Light at Night Impact
Studies have been done to test the impact dim light at night has on the ability to sleep and produce locomotor activity in rats and mice. Protocols in animals being exposed to dim light at night, during their normal dark phase, has shown to reduce locomotor activity levels, and in rats, studies show that there is a decreased amplitude of daily rhythms of REM and NREM sleep, in addition to specific changes in the NREM EEG spectra around 16-19Hz.
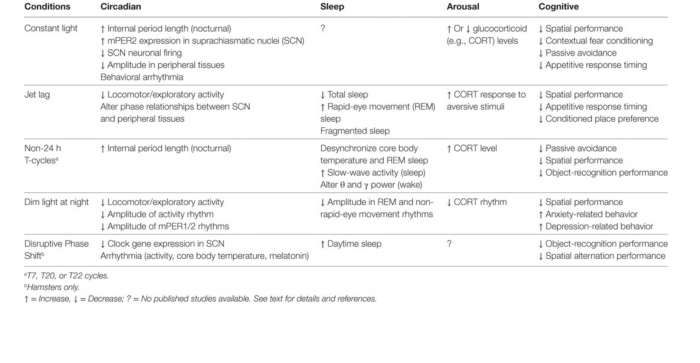
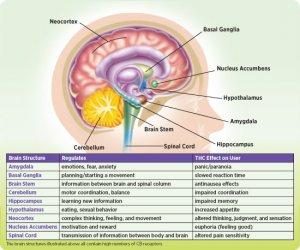
The figure below shows the impact of light (in different forms) on circadian rhythms, sleep, arousal, and cognitive function. As the figure shows, dim light at night results in a decrease in locomotor/ exploratory activity, a decrease in amplitude of activity rhythm, and a decrease in amplitude of mPER1/2 rhythms. There is also a decrease in the amplitude in REM and non-rapid eye movement rhythms. Likwise, there is also a decrease in spatial performance, and increase in both anxiety-related behavior, and depression-related behavior.
 Likewise, another study found that while any light can suppress the secretion of melatonin, specifically blue light at night will cause more of a powerful effect. It was shown that blue light suppresses melatonin about twice as long as green light, while shifting circadian rhythms twice as much.
Likewise, another study found that while any light can suppress the secretion of melatonin, specifically blue light at night will cause more of a powerful effect. It was shown that blue light suppresses melatonin about twice as long as green light, while shifting circadian rhythms twice as much.
Overall, blue light impacts our ability to get a good night’s sleep, through REM sleep, which is vital for our health and wellness. Prioritizing restful sleep through avoiding light and following our natural circadian rhythm is important for human’s health.



 By Hannah P.
By Hannah P.







 (2, 3, 4)
(2, 3, 4)