Sesame Street writer Emily Perl Kingsley is often asked to describe what it is like to raise child with disability. She describes it as planning a trip to Italy, but unexpectedly arriving in Holland. Her entire poem is moving, but she explains that while the trip was unexpected, there are still many things to enjoy about Holland.
The concept of Holland is transferrable to any parent of a child with a disability, but in this blog, we are going to dig into the Holland of Autism.
What is it like to go to Holland?

For individuals who experience autism, they can land anywhere in the spectrum where they may be met by challenges in social skills, verbal and nonverbal communication, repetitive behavior, and sometimes intellectual disabilities.
There are many guides along the way to help individuals with autism. Depending on their needs, these range from peer social interactions in the classroom to family development at home. Technology has also had an important role in reaching individuals with autism, as they may find it easier to communicate through apps on phones and tablets.
Why does Holland exist?
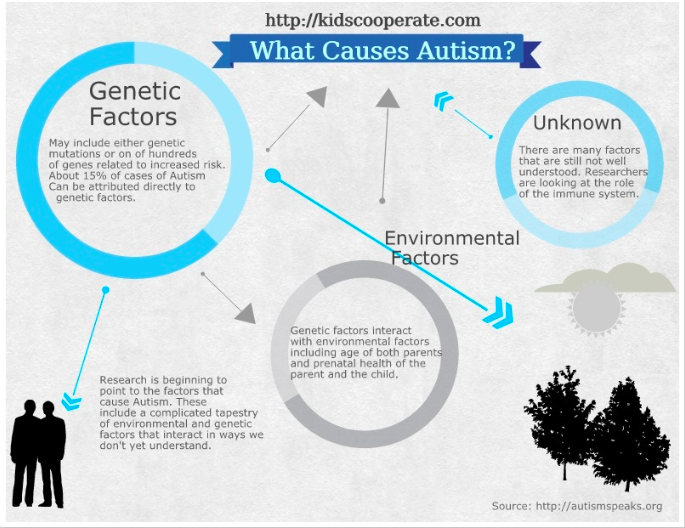
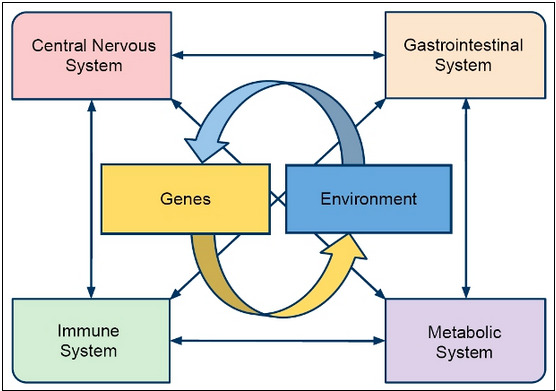
Autism is a neurological disorder that is influenced by both genetic and environmental factors. While autism-related genes are the greatest contributor, recent research has taken interest in the environmental factors that may further activate these genes.
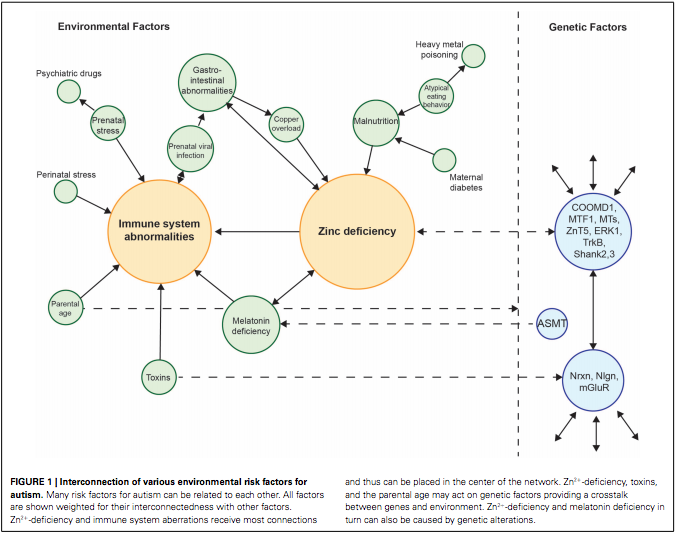
Of the many environmental factors Andreas Grabrucker proposed to have an influence on autism incidence, they could be connected into two broad categories: immune system disruptions and zinc deficiency.
Some immune system disruptions were traced back to prenatal/perinatal stress, exposure to toxins, or increased parental age. The zinc deficiency could stem from malnutrition, copper overload, or a melatonin deficiency. Interestingly, the zinc deficiency could also contribute to immune system abnormalities.
Why is zinc so important?
The presence of zinc is incredibly important to the normal function of glutamate neurons. Autism is characterized by glutamate excitotoxicity, which means that too much glutamate is being released and causes the neuron to be overactive.
Zinc normally decreases glutamate release, so when that is not present, glutamate is continually released. Zinc is also important for proper function of other receptors and the structural integrity of the neurons. If there is plenty of zinc, they are able to stack certain proteins to make the synapse of the neuron stronger.
If Holland isn’t so bad, why are we trying to fix it?

All in all, engaging a child with a disability like autism is truly a journey. Some parents may say that they would not trade this journey for anything, as the diagnosis is part of their child’s identity. However, if they were given the choice to provide their child an autism-free life, I struggle to understand how any parent would deny that of their children.
We should continue to advocate for those affected by autism. Not only to provide those individuals with the services necessary to adapt to everyday life, but to also support research in finding a cure for autism.
While a prenatal zinc tablet may not be the answer, this recent research may lead to a zinc-based treatment in the future to diminish the environmental factors on autism.
“