Neurochemistry has allowed me to integrate and apply the skills and competencies that a liberal arts education at Concordia College strives all students to meet. Learning at a liberal arts college means that the education I receive is holistic and it focuses around many areas of study in conjunction with forcing students to get out into the community to make a difference. In my well-rounded education, I was emmerssed in topics that I never would have studied before coming to college, but I am able to look at a signal topic with various lenses that my other causes have instilled in me that makes me a more intuitive person when going into the dental profession. The learning outcomes at Concordia College for the liberal education are outlined below.
Neurochemistry has allowed me to integrate and apply the skills and competencies that a liberal arts education at Concordia College strives all students to meet. Learning at a liberal arts college means that the education I receive is holistic and it focuses around many areas of study in conjunction with forcing students to get out into the community to make a difference. In my well-rounded education, I was emmerssed in topics that I never would have studied before coming to college, but I am able to look at a signal topic with various lenses that my other causes have instilled in me that makes me a more intuitive person when going into the dental profession. The learning outcomes at Concordia College for the liberal education are outlined below.
Instill a love of learning:
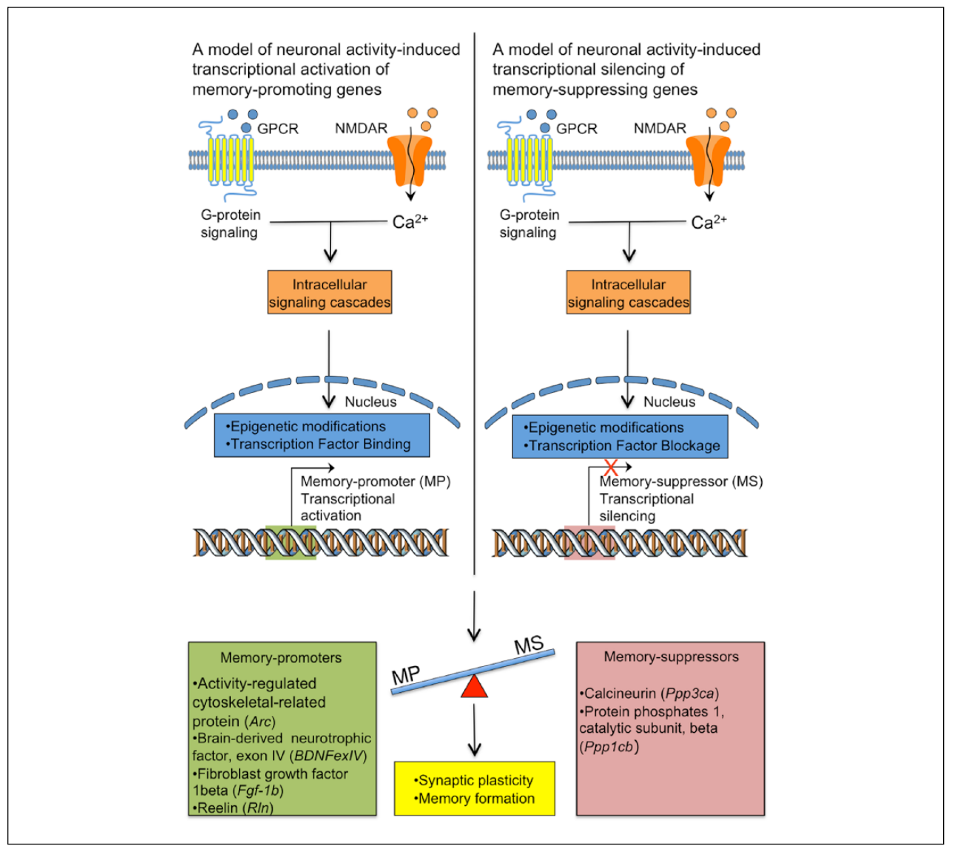
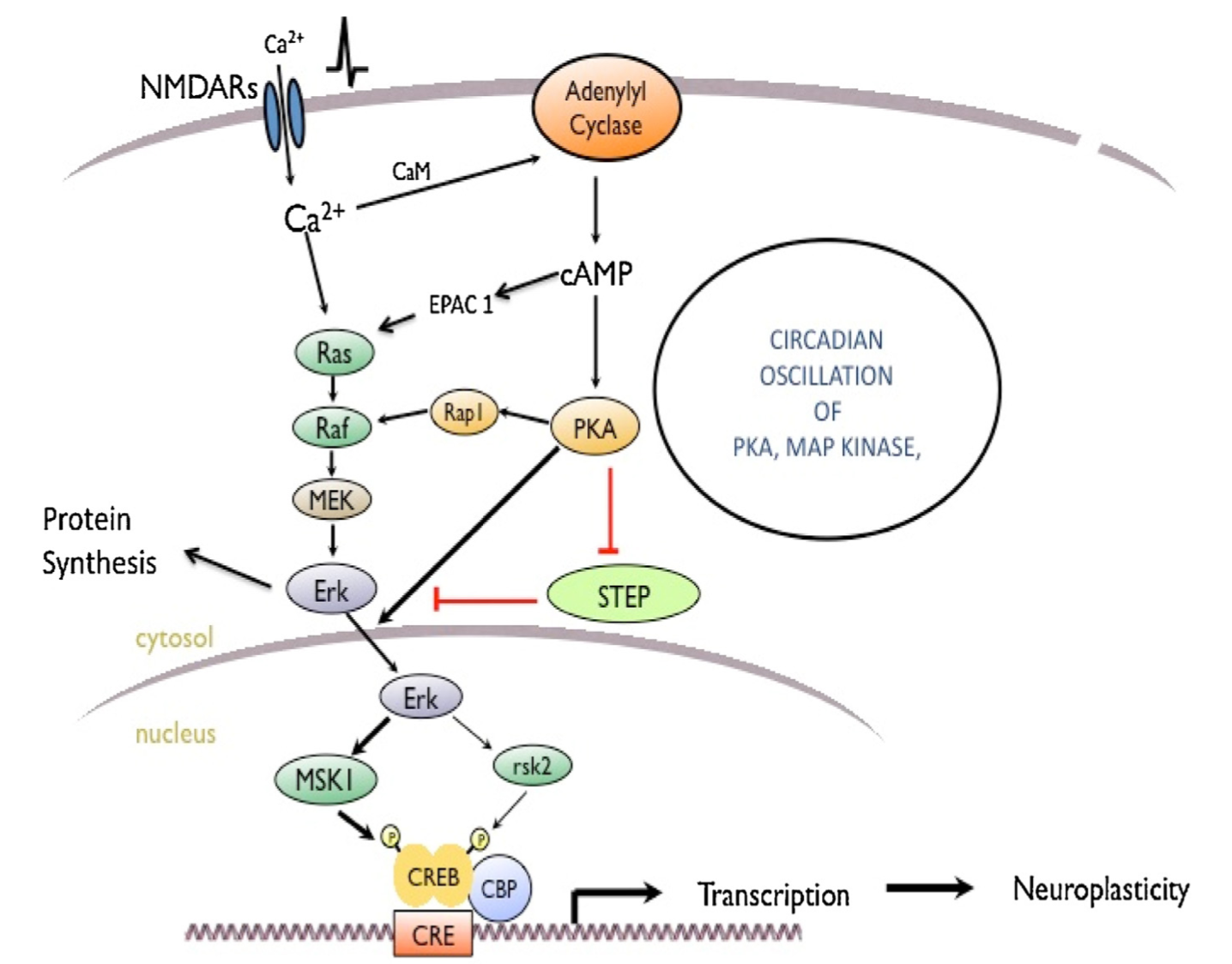
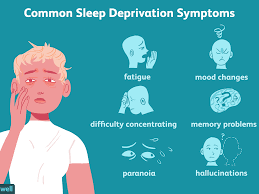
Neurochemistry has expanded upon how much knowledge within my major of neuroscience can be applied to various disease states in order to understand what is physiologically happening in the body in atypical circumstances. In many of my neurochemistry courses, we discuss what typical biochemical processes occur. Neurochemistry threw our knowledge into an application stage by applying our previous knowledge to disease states to understand what is happening within the body and what mechanisms are effected when diseases take place. By reading current research and asking questions about disease states, I have been better able to learn from my curiosity and questions about neurological diseases that many people have no idea about to understand the pathology of a disease, as well as how to prevent and ultimately treat disease states. As many of my classmates and myself are going into the sciences, I think it is important to acknowledge that we are learning to take previous knowledge to help treat or solve diseases that affect our population in order to improve the quality of life of many individuals. Not only did I improve my problem solving skills and how to better ask questions to solve, but I also learned to better communicate in writing and verbally through blog posts and our “speed” information sessions. The speed information sessions with other classmates helped me to pair down my question of interest and the information to answer the question in a few sentences, which will help me as a dental professional explaining to my patients what is happening.
Develop foundational skills and transferable intellectual capacities:
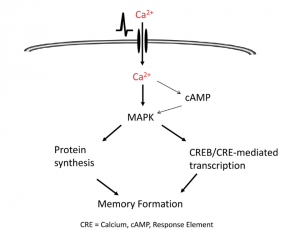
At the start of neurochemistry, the first seven class periods were on setting the foundation of common pathways in the brain that we would later cover in disease state papers. Understanding the common neurological pathways allowed me to better understand where in a pathway a disease state is dysregulated and how it impacts the rest of the typical pathway. These skills will allow me to look at current dental disease states and better understand where in the pathway select disease states the dysfunction happens. I also learned how to break down academic articles, which is necessary in the dental profession as technology and biomaterials are always changing. I would highlight the skill of making dense information understandable to my classmates and non-science individuals as a core competency on my resume. I think that this knowledge will allow me to more quickly process academic papers as a dental professional to augment my own knowledge and how to ensure that I change how I practice to support my patients and their health.
Develop an understanding of disciplinary, interdisciplinary, and intercultural perspectives and their connections:
Beyond taking courses to support my knowledge of neuroscience courses, I have also supplemented my disciplinary knowledge with interdisciplinary learning through my minors of chemistry and food/nutrition/dietetics. My knowledge of chemistry and nutrition have given be a broader view of neurological disease states. I bring my passion for nutrition into the course by wanting to better understand what the role of nutrition is in the progression or treatment of neurological disease. One example of problem solving using my science perspectives includes how maternal nutrition can impact the risk of having offspring with autism. I found that increasing omega-3 fatty acid, vitamin D, iron, and folate consumption in pregnant women can significantly decrease the risk of having a child with autism through various pathways to promote healthy offspring. The intercultural component of the puzzle can be found in looking at what other countries do to promote or prevent diseases along with speaking to my classmates to learn about how their experience shapes their knowledge and overall perspective that they bring to class. Having discussion days in class better allows me to ask students why they believe what they do and learn from their experience to have a better knowledge base and become a more well-rounded individual.
Cultivate an examined cultural, ethical, physical and spiritual self-understanding:
During discussion days, I learned from my classmates about their own culture, ethical, physical, and spititual knowledge and believes when ethical questions were posed about how to combat and treat disease, as well as the best options on how to help people with disease states. By just listening, I acknowledged how my beliefs and perspectives also shaped my own beliefs while making room for others to share their understanding. I did not quite understand how my beliefs and attitudes could slightly change by just having a conversation with others weekly.
Encourage responsible participation in the world:
I did not do the PEAK project this year, but I think that learning about disease states and helping others who are neurologically different can raise awareness and even understanding about the human condition. I think this skill can help me as a dental professional when I see clients who are neurologically diverse to treat everyone the same, with respect and kindness.
Conclusion:
Being able to use my liberal arts education to make me a more well-rounded student has been amplified in my neurochemistry course as I have brought many of the components together throughout the course this semester. I am so excited to use this knowledge in dental school next year and in my career as a dentist.