With one in every five Americans experiencing a mental illness at some point in their lives, how is it that the stigma surrounding mental illness remains so pervasive? Despite the high societal prevalence, according to National Alliance on Mental Illness (NAMI), almost 57% of adults with mental illness do not receive treatment and the average delay between symptom onset and treatment is eleven years. For Karen Ranus, Executive Director of NAMI-Austin, it comes down to a disconnect between viewing mental health conditions as medical conditions because parts of society view mental illnesses as “some character flaw or some kind of moral failing… a personality flaw.” Clearly, linking mental illness with moral failings contributes to and perpetuates the existing stigma surrounding mental health.
So, how do we begin unlinking mental illness and moral failures?
According to NAMI, talking openly about mental health and educating both yourself and others are two incredibly important ways to help decrease the stigma surrounding mental health. So, let’s take a quick dive into the brain and look at one of the biological risk factors for developing schizophrenia.
Inside the brain:
One of the ways that your body seeks to be more efficient is by having multiple copies of a gene arranged in sequence one right after another along the same strand of DNA. This is a really powerful way for your body to make multiple RNA copies of those genes by having RNA Polymerase, the molecular machine that transcribes DNA into RNA, simply bind at the beginning of that series of genes and work down the DNA strand at one time, rather than having to bind multiple times to the start of the gene to make the same number of RNA copies. After this process of transcription is completed, the RNA will be translated into proteins by another molecular pathway. While we won’t spend time on translation here, you should know that more copies of RNA transcripts usually result in more proteins being formed. (If you want to learn more about transcription and translation, click here.)

(image credit: Khan Academy)
Interestingly, the number of these gene copies can vary from person to person. This is called Copy Number Variation or CNV. Importantly, CNVs can be passed from parents to children. In schizophrenia, specific CNVs at different locations on chromosomes are associated with a higher risk of developing the illness. This is an exciting area of active research in genetics because we do not yet understand the exact molecular pathway between the genetic risk factor posed by the CNV and the development of schizophrenia symptoms. (Image Credit: National Institutes of Health)

Now that we understand one of the biological risk factors for schizophrenia development, what else should we do to help end the stigma surrounding mental illness? NAMI’s other recommendations are:
- Be conscious of the language we use to describe mental health conditions
- Encourage equality between physical and mental illness
- Show compassion for those with mental illness
- Choose empowerment over shame
- Be honest about treatment
- Let the media know when they’re being stigmatizing
- Don’t harbor self-stigma
To learn more about mental health stigma and take NAMI’s StigmaFree pledge, click here.



 been shown to be involved with schizophrenia is the Wnt signaling pathway. When the Wnt pathway is activated it induces a cascade of events that can effect nervous system functions including neural circuit formation and synaptic
been shown to be involved with schizophrenia is the Wnt signaling pathway. When the Wnt pathway is activated it induces a cascade of events that can effect nervous system functions including neural circuit formation and synaptic 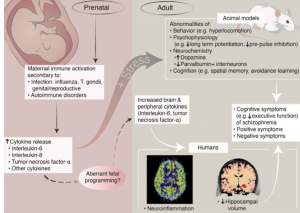 body can recruit inflammation-induced cytokines. There has been research that shows mothers who have birthed children who later are diagnosed with schizophrenia have been noted to have an elevation by nearly twofold of cytokine family molecules. Specifically, the most common cytokine family molecules that have been studied are interleukin-8 (IL8), interleukin-6 (IL6), tumor necrosis factor alpha (TNFalpha), as well as others. These molecules are soluble peptides that can cause decrease brain development and behavior abnormalities, and they have been correlated to decrease cerebral cortical neuron survival especially during brain
body can recruit inflammation-induced cytokines. There has been research that shows mothers who have birthed children who later are diagnosed with schizophrenia have been noted to have an elevation by nearly twofold of cytokine family molecules. Specifically, the most common cytokine family molecules that have been studied are interleukin-8 (IL8), interleukin-6 (IL6), tumor necrosis factor alpha (TNFalpha), as well as others. These molecules are soluble peptides that can cause decrease brain development and behavior abnormalities, and they have been correlated to decrease cerebral cortical neuron survival especially during brain 
 Lithium (yes, the element, in pill form) has been used as a treatment for schizophrenia since at least the late 19th century. It didn’t become a scientifically-based treatment until 1949, and then took another 20 years to get approval from the FDA. The fact that it wasn’t scientifically recognized didn’t stop it from being an effective treatment well before 1949 though, and amazingly, it is still used to this day as one of the most effective treatments for schizophrenia.
Lithium (yes, the element, in pill form) has been used as a treatment for schizophrenia since at least the late 19th century. It didn’t become a scientifically-based treatment until 1949, and then took another 20 years to get approval from the FDA. The fact that it wasn’t scientifically recognized didn’t stop it from being an effective treatment well before 1949 though, and amazingly, it is still used to this day as one of the most effective treatments for schizophrenia.





 disorders involving the brain. At first glance, the two seem strikingly different: when we think of symptoms of schizophrenia, we may think of hallucinations, delusions, or loss of speech and movement. With ASD, we may think of interrupted social and communication skills or repetitive behaviors. ASD is typically evident and diagnosed in childhood, while schizophrenia often doesn’t show up for several decades of a person’s life. However, the two disorders arise from similar molecular causes and even their symptoms are more alike than you might realize.
disorders involving the brain. At first glance, the two seem strikingly different: when we think of symptoms of schizophrenia, we may think of hallucinations, delusions, or loss of speech and movement. With ASD, we may think of interrupted social and communication skills or repetitive behaviors. ASD is typically evident and diagnosed in childhood, while schizophrenia often doesn’t show up for several decades of a person’s life. However, the two disorders arise from similar molecular causes and even their symptoms are more alike than you might realize. What about ASD?
What about ASD?
 voices are most often hostile and scary, but different cultures see those voices as friendly and possibly even magical.
voices are most often hostile and scary, but different cultures see those voices as friendly and possibly even magical.